Author Interviews, Endocrinology, Thyroid Disease / 11.06.2020
Thyroid Eye Disease Can Have Long Term Impact on Vision, Eye Appearance and Quality of Life
MedicalResearch.com Interview with:
 Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
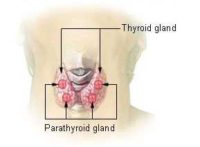
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
 Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)