Author Interviews, Opiods, Pediatrics, Surgical Research / 09.08.2019
Tonsillectomy: Over Half of Children Have Opioid Prescription Filled
MedicalResearch.com Interview with:
Kao-Ping Chua, M.D., Ph.D.
Assistant Professor,
Department of Pediatrics and Communicable Diseases
Susan B. Meister Child Health Evaluation and Research Center
University of Michigan
Ann Arbor, Michigan
MedicalResearch.com: What is the background for this study?
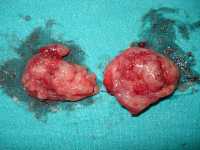
Response: Tonsillectomy is one of the most common surgeries performed in children. It is also one of the most common reasons children are prescribed opioids, even though randomized trials suggest that non-opioids like ibuprofen are equally effective for pain control. We were interested in understanding whether it is possible to safely reduce opioid exposure after tonsillectomy in children without increasing the risk of complications such as emergency department visits for uncontrolled throat pain, which could lead to dehydration.
(more…)