25 Apr Breast Cancer Screening: One-Size-Fits-All Approach May Not be Optimal, Equitable or Fair
MedicalResearch.com Interview with:

Dr. Fallah
Mahdi Fallah, MD, PhD
Study and Group Leader
Risk Adapted Prevention (RAD) Group
Division of Preventive Oncology
National Center for Tumor Diseases (NCT)
German Cancer Research Center (DKFZ)
Heidelberg, Germany
MedicalResearch.com: What is the background for this study?
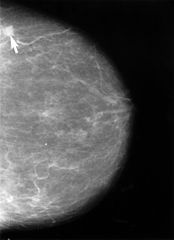
Response: Breast cancer is a significant public health problem, being the most commonly diagnosed cancer and the second leading cause of cancer death in women in the US. Breast cancer screening from age 50 has been associated with a reduction in mortality and is recommended by the US Preventive Services Task Force. However, there is a significant disparity in mortality rates between Black and White individuals, with Black women having a higher death rate, especially before age 50. The current one-size-fits-all policy for breast cancer screening may not be equitable or optimal, and risk-adapted starting ages of screening based on known risk factors, such as race and ethnicity, may be recommended to optimize the benefit of screening. Our study aimed to provide evidence for a risk-adapted starting age of screening by race and ethnicity.
MedicalResearch.com: What are the main findings?
Response: Our main finding suggests that with current recommendation of starting breast cancer screening for all from age 50, Black females should start breast cancer screening 8 years earlier than the general female population, at age 42 years, while other populations, such as White females, should start screening later, at age 51 years. American Indian or Alaska Native and Hispanic females should start at age 57 years and Asian or Pacific Islander females at age 61 years. If breast cancer screening was supposed to start at age 45 years for all US women, Black females should start screening at age 38 years, non-Hispanic White females at age 46 years, Hispanic females at age 49 years, Asian and Pacific Islander females at age 50 years, and American Indian or Alaska Native females at age 51 years. If breast cancer screening was supposed to start at age 40 years for the entire female population, Black females should start it at age 34 years, White females at age 41 years, Hispanic females at age 43 years, and American Indian or Alaska Native and Asian or Pacific Islander females at age 43 years.
MedicalResearch.com: What should readers take away from your report?
Response: Readers should take away that the one-size-fits-all approach to breast cancer screening may not be optimal, equitable, or fair, and that a risk-adapted approach based on race and ethnicity may provide better outcomes in addressing mortality rates among different populations. Health policy makers and clinicians should consider adopting this approach to improve the efficacy of breast cancer screening and optimize resource allocation.
MedicalResearch.com: What recommendations do you have for future research as a results of this study?
Response: Future research could explore the reasons why different races and ethnicities have different breast cancer mortality rates, including genetic, socioeconomic, and lifestyle factors. Such research can help develop more targeted and effective screening methods to further reduce breast cancer mortality rates and its disparity by race and ethnicity.
MedicalResearch.com: Is there anything else you would like to add? Any disclosures?
Response: There is a tendency among medical societies to lower the age of breast cancer screening for all women from 50 to 45 or even 40 years. Lowering the starting age for “all” women to younger ages may not be effective and may harm those at low risk. Instead, it would be more equitable to screen high-risk women earlier and low-risk women later. Asian or Pacific Islander women, as well as Hispanic and American Indian or Alaska Native women, have a lower risk of breast cancer and mortality, and screening them as early and as often as other women may cause more harm than good. Overdiagnosis and overtreatment resulting from unnecessary early screening can cause physical and emotional harm, lead to increased healthcare costs, and potential loss of income due to treatment-related time off work. Research on this issue is crucial to optimize the benefits of screening while minimizing harm.
Nothing to disclose.
Citation:
Chen T, Kharazmi E, Fallah M. Race and Ethnicity–Adjusted Age Recommendation for Initiating Breast Cancer Screening. JAMA Netw Open. 2023;6(4):e238893. doi:10.1001/jamanetworkopen.2023.8893
https://pubmed.ncbi.nlm.nih.gov/37074714/
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on April 25, 2023 by Marie Benz
