Author Interviews, JAMA, OBGYNE, Pediatrics, USPSTF / 09.08.2023
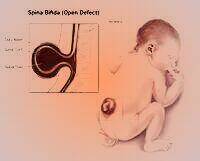
USPSTF: Anyone Who Could Become Pregnant Should Take Folic Acid To Prevent Spinal Cord Defects
MedicalResearch.com Interview with:x
Wanda K. Nicholson, M.D., M.P.H., M.B.A.
Senior Associate Dean for Diversity, Equity, and Inclusion
Professor of Prevention and Community Health
Milken Institute School of Public Health
George Washington University
Vice chair of the U.S. Preventive Services Task Force
MedicalResearch.com: What is the background for this study?
Response: Neural tube defects are when a baby’s spinal cord or brain don’t develop properly during pregnancy, which can cause serious complications including disability and death. The good news is that taking folic acid supplements before and during early pregnancy is proven to help prevent this from happening.
(more…)