Author Interviews, Heart Disease, JACC, Surgical Research / 22.05.2023
Novel Coating on Investigational WATCHMAN FLX™ Pro device May Reduce Risk of Embolism
MedicalResearch.com Interview with:
Aloke V. Finn MD
Medical Director/Chief Scientific Officer
CVPath Institute Inc.
Gaithersburg, MD 20878
MedicalResearch.com: What is the background for this study?
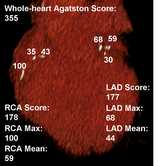
Response:Transcatheter left atrial appendageal closure (LAAC) has become an established therapeutic approach for prevention of stroke in subjects with non-valvular atrial fibrillation who are ineligible for long-term oral anticoagulation. Device-related thrombus (DRT), developing after LAAO procedures occurs in a small proportion but patients receiving these devices but is associated with critical embolic events such as ischemic stroke. Thrombogenicity and delayed endothelialization of fabric play a role in the development of DRT. Fluorinated polymers are known to have thromboresistant properties which may favorably modify blood biomaterial interactions of a LAAO device.
In this study we compared the thrombogenicity and endothelial coverage (EC) after left atrial appendage occlusion (LAAO) between a novel fluoropolymer-coated Watchman (FP-WM (Watchman FLX PRO) and the conventional uncoated Watchman FLX (WM).
(more…)