20 Nov Skin Conditions Associated with Down Syndrome
MedicalResearch.com Interview with:
Dr. Rork
Jillian F. Rork, MD
Assistant Professor of Dermatology
Dartmouth-Hitchcock Medical Center at Manchester and
The Geisel School of Medicine
Society for Pediatric Dermatology Member
MedicalResearch.com: What is the background for this study? Would you briefly explain the genetic condition of Down syndrome?
Response: Down syndrome is the most common chromosomal abnormality, occurring in approximately 1 in 700 newborns in the United States. Trisomy of chromosome 21 can result in multisystem involvement such as hearing loss, heart defects, autoimmune conditions and dementia.
This study focuses on how trisomy 21 affects one of the body’s largest organs, the skin. Current literature addressing dermatologic conditions associated with Down syndrome is limited. There is often emphasis on rare skin conditions such as elastosis perforans serpiginosa, milia-like idiopathic calcinosis cutis, and eruptive syringomas. There is lack of consensus on incidence of more common disorders. We performed a retrospective chart review of 101 patients with Down syndrome in our dermatology practice at the University of Massachusetts to better describe associated skin conditions.
MedicalResearch.com: What are the main dermatologic conditions affecting this syndrome?
Response: Dermatologic conditions in patients with Down syndrome vary by age, but are most often adnexal, eczematous, and autoimmune. Folliculitis, especially on the buttocks and thighs, was the most common diagnosis overall (30.7%), followed by seborrheic dermatitis (26.7%) and hidradenitis suppurativa (22.8%).
Folliculitis and hidradenitis suppurativa are likely on the same continuum in Down syndrome; in fact, approximately 40% of patients with folliculitis also had hidradenitis. Our findings also support other recent studies showing an increased prevalence of hidradenitis in patients with Down syndrome. The genetic abnormalities of trisomy 21 could predispose to the development of adnexal conditions including increased amyloid precursor protein and defective Notch signaling.
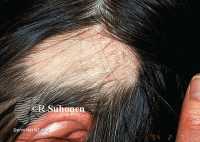
Example of Alopecia Areata DermNetNZ
Alopecia areata, an autoimmune form of hair loss, occurs more often in Down syndrome. Our findings support previous studies showing that alopecia areata associated with Down syndrome tends to present earlier in life and more commonly affect males. It is well recognized that autoimmune disease occurs more often in patients with Down syndrome, including hypothyroidism and celiac disease. This is likely secondary to widespread immune dysregulation including interferon-gamma hyperactivity and trisomy of the AIRE (autoimmune regulator) gene located on chromosome 21. Interestingly, both of these mechanisms are important in the pathogenesis of alopecia areata. When the diagnosis of alopecia areata is made in a patient with Down syndrome, providers should confirm TSH screening is up-to-date as alopecia areata can be associated with hypothyroidism.
Seborrheic dermatitis was the most common eczematous condition followed by xerosis. Dermatophyte infections such as onychomycosis were the most common skin infection and occurred in several pediatric patients.
Psoriasis was present in nine patients. It is unclear whether there is a potential association between psoriasis and Down syndrome. This could be secondary to T-cell dysfunction and interferon-gamma. More research is needed in this area.
Lastly, we did report two cases of cutaneous malignancy, including a basal cell carcinoma and melanoma in-situ. As life expectancy in Down syndrome increases, annual skin examinations should be encouraged.
MedicalResearch.com: What should readers take away from your report?
Response: Dermatologic conditions in patients with Down syndrome vary by age, but are most often adnexal, eczematous, and autoimmune. This recognition could help clinicians not only anticipate diagnoses, but also provide bench to bedside correlations between the skin, trisomy 21, and resulting downstream effects on the immune system.
MedicalResearch.com: What recommendations do you have for future research as a result of this study?
Response: We need more descriptive studies on many of these diagnoses to better define their phenotype in Down syndrome. We need to collaborate with basic scientists to explore the pathogenesis behind these associations; this could provide further insight into disease mechanism and potential treatments.
MedicalResearch.com: Is there anything else you would like to add? Any disclosures?
Response: I would like to thank my research mentors, Dr. Leah Belazarian and Dr. Karen Wiss. I would also like to thank all of my patients and colleagues in the Down syndrome community who are helping us learn more about the skin and Down syndrome.
Citation:
Rork, JF, McCormack, L, Lal, K, Wiss, K, Belazarian, L. Dermatologic conditions in Down syndrome: A single‐center retrospective chart review. Pediatr Dermatol. 2020; 37: 811– 816. https://doi.org/10.1111/pde.14214
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on November 20, 2020 by Marie Benz MD FAAD
