09 Nov Tonsillectomy Often Done When Not Indicated (and vice versa!)
MedicalResearch.com Interview with:
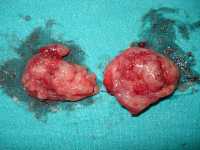
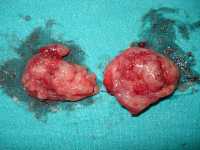
A pair of tonsils after surgical removal
Wikipedia image
Tom Marshall, MSc, PhD, MRCGP, FFPH
Professor of public health and primary care
Institute of Applied Health Research
University of Birmingham, Birmingham, UK
MedicalResearch.com: What is the background for this study?
Response: Tonsillectomy is one of the most common childhood surgical procedures. There are two main indications: recurrent sore throat and sleep-related breathing problems (including obstructive sleep apnoea).
Jack Paradise’s 1984 study made clear tonsillectomy is modestly effective in children with frequent, severe sore throats: seven in one year, or five yearly in two successive years, or three yearly in three successive years. Sore throats must have symptoms: fever, pus seen on tonsils, lymphadenopathy or confirmed Streptococcal infection. With surgery, children average two sore throats in the next year, without surgery, three. Two years later there is no difference. Further research shows the benefits are too tiny to justify surgery in children with less frequent, less severe or undocumented sore throats. Subsequent randomised controlled trials have not changed the evidence. There isn’t enough good evidence to support surgery in children with obstructive sleep apnoea or sleep related breathing problems.
Tonsillectomy is not a trivial procedure, about 2% are readmitted with haemorrhage and about 1 in 40,000 dies. Childhood tonsillectomy is linked to risk of adult autoimmune diseases. It is important to be sure tonsillectomy is only undertaken in children where there are evidence-based indications.
MedicalResearch.com: What are the main findings?
Response: We looked at the medical records of 1.63 million UK children, between 2005 and 2016. We found 18,281 children who underwent tonsillectomy but only 2,144 (11.7%) had evidence-based indications. Most childhood tonsillectomies were for sore throats, but too few to justify surgery; 12.3% were for sleep disordered breathing; 3.9% were for obstructive sleep apnoea. The pattern of indications for tonsillectomy was similar to that reported by the Royal College of Surgeons of England.
At the same time we found 15,760 with evidence-based indications, meaning only 13.6% (2,144) underwent surgery. We also found that of 15,205 children with sleep related breathing problems, only 14.8% underwent tonsillectomy and of 3,185 children with obstructive sleep apnoea, only 22.2%. There was little change over 12 years except for an increase in tonsillectomies for obstructive sleep apnoea.
MedicalResearch.com: What should readers take away from your report?
Response: Most children undergoing tonsillectomy do not benefit enough to justify surgery. This is because most are undertaken in children who do not meet evidence-based criteria. Most children who do meet evidence-based criteria don’t ever have their tonsils removed.
Parents should be given accurate honest information on the benefits and hazards of tonsillectomy so they can make an informed decision. Parents can be reassured that the vast majority of children with frequent severe sore throats do not undergo tonsillectomy, therefore surgery is not essential.
Parents should be told that there is insufficient evidence surgery is effective for obstructive sleep apnoea or other sleep related breathing problems and can be reassured that the vast majority of children with either condition do not undergo tonsillectomy, therefore surgery is not essential.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: There are huge international and regional variations in tonsillectomy rates. Rates in the USA, Norway, Netherlands are over twice those in the UK. Rates in Spain, Portugal and Poland, half those in the UK. Similar analysis of the pattern of indications for tonsillectomy should be undertaken in countries with higher and lower rates of tonsillectomy. Accurate estimates of adverse effects and mortality following tonsillectomy should be provided for parents and clinicians. The long-term safety of tonsillectomy should be investigated.
Disclosures: I have no conflicts of interest in relation to this research. In particular I derive no income or research funding from either undertaking tonsillectomies, increasing the numbers of tonsillectomies undertaken or reducing the numbers of tonsillectomies undertaken in the UK or elsewhere.
Citation:
Dana Šumilo, Linda Nichols, Ronan Ryan, Tom Marshall. Incidence of indications for tonsillectomy and frequency of evidence-based surgery: a 12-year retrospective cohort study of primary care electronic records. British Journal of General Practice, 2018; bjgp18X699833 DOI: 3399/bjgp18X699833
[wysija_form id=”3″]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on November 9, 2018 by Marie Benz MD FAAD
