
17 Oct The Role of Biomarkers in Personalized Medicine

Key Takeaways
- Biomarkers are measurable biological indicators that can help in diagnosing diseases, predicting disease progression, and guiding treatment decisions.
- They are essential for personalized medicine, allowing treatments to be tailored specifically to an individual’s biological profile.
- Targeted therapies and early detection of diseases, especially in cancer treatment, have greatly benefited from biomarker research.
- Tools like Western blotting and ELISA are commonly used to detect and analyze biomarkers, contributing to more precise medical decisions.
- While challenges exist, including cost and ethical concerns, biomarkers are paving the way for more accurate and effective healthcare.
Introduction
Personalized medicine is a new approach that focuses on providing treatments specifically designed for each patient based on their unique biological makeup. This concept is changing the way doctors treat patients by moving away from general treatments that work for the average person. Instead, doctors can now use information from biomarkers—biological molecules that offer insights into a person’s health. This allows healthcare providers to make more precise decisions about the best treatments for each individual.
In this article, we’ll dive deeper into what biomarkers are, how they work in personalized medicine, and why they are becoming essential tools in modern healthcare.
What Are Biomarkers?
Biomarkers are specific molecules found in your body—such as in blood, urine, or tissues—that can give clues about your health. These molecules are used by doctors to measure whether something in your body is working as it should, or if there’s a sign of disease. Biomarkers can help with early detection, diagnosis, and monitoring of diseases, as well as in predicting how a patient might respond to a treatment.
Biomarkers come in several forms, including:
- Diagnostic biomarkers: Used to identify the presence of a disease. For example, measuring blood sugar levels is a biomarker used in diagnosing diabetes.
- Prognostic biomarkers: These help predict how a disease might progress. For example, certain proteins in cancer patients can indicate whether their cancer is likely to spread or stay localized.
- Predictive biomarkers: These help doctors determine which treatments will work best for a patient. For instance, genetic markers may show that a person will respond well to a specific drug.
Using biomarkers, healthcare providers can tailor treatments to suit the needs of each individual, making medical care more personalized and effective.
The Influence of Biomarkers in Personalized Medicine
The use of biomarkers in personalized medicine is all about matching the right treatment to the right patient at the right time. Traditional treatments are designed to work for the majority of people, but not everyone responds to medications in the same way. Biomarkers help doctors figure out which treatments will be most effective for a specific person based on their unique biology.
1. Targeted Therapies
One of the most significant benefits of biomarkers is their ability to guide targeted therapies. These are treatments that directly attack specific aspects of a disease based on the individual’s biomarker profile. A well-known example is the treatment of HER2-positive breast cancer. HER2 is a protein found on some cancer cells, and by identifying the presence of this protein through biomarkers, doctors can prescribe drugs that specifically target HER2-positive cells, making the treatment much more effective for those patients.
Targeted therapies reduce the trial-and-error approach common in traditional medicine, improving treatment success rates while minimizing side effects. Biomarkers allow doctors to focus on the parts of the disease that matter most for each patient, ensuring that treatment is more precise.
2. Early Detection of Diseases
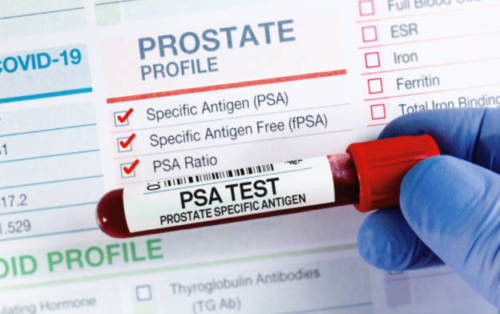
Early detection of diseases is key to improving survival rates and outcomes. Biomarkers play a vital role in catching diseases early, sometimes even before symptoms appear. For example, prostate-specific antigen (PSA) is a biomarker used to detect prostate cancer at an early stage. Early detection means that doctors can start treatment sooner, potentially halting the disease before it progresses.
Another example is the use of biomarkers in detecting heart disease. Certain proteins found in the blood can signal the early stages of heart damage, allowing for earlier interventions that could prevent a heart attack. This proactive approach to healthcare is what makes biomarkers so powerful in personalized medicine.
3. Tailoring Treatment Plans
Biomarkers also help tailor treatment plans by predicting how well a person will respond to a specific medication. For example, in cancer treatments, biomarkers can identify whether a patient is likely to benefit from chemotherapy or if a different therapy would be more effective. This means patients receive the most suitable treatment right from the start, reducing the chances of unnecessary side effects and ineffective treatments.
This personalized approach not only improves patient outcomes but also cuts down on healthcare costs by avoiding treatments that aren’t likely to work. Over time, more patients will receive treatments that are specifically designed for their condition, leading to better overall healthcare results.
Biomarkers in Cancer Treatment
Cancer research has made great progress thanks to the discovery of biomarkers. In the past, many cancer treatments were generalized, meaning that all patients with the same type of cancer received similar treatments. However, not all cancers respond the same way to treatment. Biomarkers help identify the specific characteristics of each patient’s cancer, allowing for more customized treatment.
For example, mutations in the EGFR gene are common in lung cancer patients. By detecting these mutations through biomarkers, doctors can prescribe drugs that specifically target these mutated genes, improving treatment success. Similarly, the BRCA gene mutation in breast cancer patients helps guide the decision on whether patients should undergo preventative treatments or more aggressive therapies.
Western blot labs are frequently used in this type of cancer research to measure protein levels in cancer cells. This helps scientists and doctors understand how cancer cells behave and which treatments might work best.
Challenges and Opportunities in Biomarker Research
While the use of biomarkers in personalized medicine holds great promise, there are several challenges that must be addressed:
- Validation and Accuracy: Before biomarkers can be widely used, they must be thoroughly tested to ensure they are accurate and reliable. This validation process takes time, as researchers must confirm that the biomarker consistently provides correct information.
- Cost of Testing: Advanced testing techniques, including biomarker analysis, can be expensive. This may limit access for some patients, especially in countries where healthcare resources are limited. Reducing the cost of these tests will be important for expanding personalized medicine.
- Ethical Concerns: The use of genetic information, including biomarkers, raises ethical questions. How will this data be used? Could it be misused to discriminate against patients? Ensuring patient privacy and ethical use of biomarker data will be crucial as this field grows.
Despite these challenges, advances in technology are helping to improve the reliability and accessibility of biomarker testing, opening the door for even broader use in healthcare.
Tools for Biomarker Detection
Detecting and analyzing biomarkers requires sophisticated tools. One commonly used method is Western blotting, which is a laboratory technique used to detect specific proteins in a tissue sample. This method is particularly useful in cancer research, where it can help identify protein biomarkers linked to the disease. Similarly, cell panel screening services play a crucial role in testing multiple cell types to analyze how they respond to different therapies, further enhancing personalized treatment strategies.
Another valuable tool is the ELISA (Enzyme-Linked Immunosorbent Assay), which helps detect the concentration of biomarkers in body fluids like blood or urine. ELISA tests are widely used in diagnostics to measure proteins, hormones, or other substances that act as biomarkers.
These tools, along with emerging technologies, are making it easier to identify and study biomarkers, which in turn helps improve the precision of personalized treatments.
Conclusion
Biomarkers are becoming essential tools in the advancement of personalized medicine. By providing detailed insights into a patient’s health, biomarkers help doctors make more informed decisions about diagnosis, treatment, and disease prevention. As research advances and biomarkers become more widely used, we’re likely to see even greater benefits in personalized healthcare, resulting in better outcomes for patients everywhere.
About the Author:

Dr. Steven Xia
Steven Xia, PhD is a passionate histologist and founder of Boster Bio in 1993, overcame humble beginnings in a rural farming community to become the first in his village to earn a PhD. Driven by a vision to support China’s medical and research community in the early ’90s, he started developing proprietary reagents for histology in a small room with minimal resources. Today, Boster Bio reflects his dedication and innovation, providing high-sensitivity ELISA kits and antibodies that empower researchers globally.
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Do not delay medical treatment because of information obtained from this site.
Some links are sponsored. Product, services and providers are not vetted, warranted or endorsed.
Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on October 17, 2024 by Marie Benz MD FAAD
