MedicalResearch.com Interview with:
 Kathleen Squires MD
Kathleen Squires MD
Director, Division of Infectious Diseases
Jefferson University Hospitals and
Ming-Tai Lai, PhD
Senior Principal Scientist, Biology Discover
Merck
MedicalResearch.com: What is the background for this study? What are the main findings?
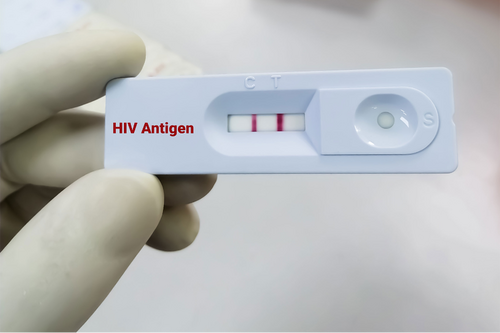
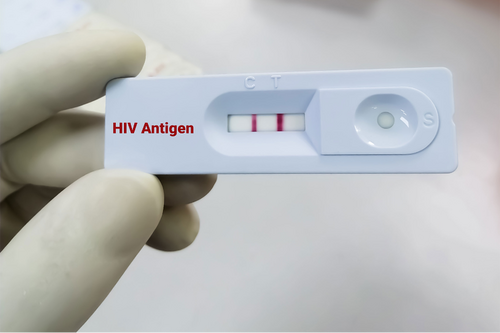
Dr. Squires: The DRIVE-FORWARD study is a pivotal, randomized, double-blind, Phase 3 study that evaluated the safety and efficacy of doravirine (DOR), a non-nucleoside reverse transcriptase inhibitor (NNRTI) in treatment-naïve adults with HIV-1 infection. Data from week 48 of this trial have previously been presented demonstrating that doravirine met its primary endpoint of non-inferior efficacy compared to ritonavir-boosted darunavir (DRV+r). In addition, at 48 weeks, a secondary endpoint showed that the doravirine-treated group had statistically significant lower levels of fasting LDL-C and non-HDL-C versus the DRV+r group.
The data presented at AIDS 2018 are week 96 data from the DRIVE-FORWARD trial.
At week 96, the doravirine group demonstrated efficacy of 73.1% compared with 66.0% in the DRV+r group, a treatment difference of 7.1% (95% CI: 0.5, 13.7) Two participants in the DOR treatment group developed genotypic and phenotypic resistance to DOR through 96 weeks of treatment. The rate of discontinuation of therapy due to adverse events was 1.6 percent in the DOR group and 3.4 percent in the DRV+r group.
Doravirine is a late-stage investigational NNRTI for the treatment of HIV-1 infection in treatment-naïve adults and is being evaluated both as a once-daily single-entity tablet in combination with other antiretroviral agents, and as a once-daily fixed-dose combination regimen with lamivudine (3TC) and tenofovir disoproxil fumarate (TDF). Earlier this year, Merck announced that the FDA accepted for review two New Drug Applications (NDAs) for doravirine for the treatment of HIV-1 infection in treatment-naïve adults. The NDAs are based upon the findings at week 48 of two ongoing Phase 3 trials, DRIVE-FORWARD and DRIVE-AHEAD, evaluating the efficacy and safety of doravirine and the fixed-dose combination regimen of DOR/3TC/TDF, respectively. The FDA has set a target action date of October 23, 2018 for both applications.
Dr. Lai: This study aimed to characterize the mutant viruses selected in treatment-naïve participants through week 48 from DRIVE-FORWARD and DRIVE-AHEAD, and to assess the impact of selected mutations on non-nucleoside reverse transcriptase inhibitor (NNRTI) susceptibility and viral fitness. All of the seven doravirine (DOR)-resistant mutants are either partially susceptible or susceptible to etravirine. Mutants containing the F227C substitution were shown to be hypersusceptible to some nucleoside reverse transcriptase inhibitors (NRTIs) such as azidothymidine (AZT), tenofovir (TFV), lamivudine (3TC), and MK-8591. Among the 12 participants who developed efavirenz (EFV) resistance, 9 of the EFV-resistant clinical mutants were susceptible to DOR with fold-change <2.5.
The majority of DOR-selected viruses identified in the treatment-naïve participants in clinical trials to date retain susceptibility to etravirine and hypersensitivity to some NRTIs, with low replication capacity. In addition, the majority of EFV-selected viruses retain susceptibility to DOR.
(more…)