Author Interviews, Infections, NEJM, STD / 06.03.2025
NEJM: Treating Male Partners Reduces Recurrence Rate of Bacterial Vaginosis
MedicalResearch.com Interview with:
Lenka Vodstrcil PhD
Senior Research Fellow
Deputy Head, Genital Microbiota and Mycoplasma Group
President, Sexual Health Society of Victoria
Associate Editor, Sexually Transmitted Infections
School of Translational Medicine, FMNHS, Monash University
Melbourne Sexual Health Centre, The Alfred Hospital
Melbourne School of Population & Global Health, University of Melbourne
Catriona Bradshaw MMBS(Hons), PhD, FAChSHM, FAHMS
Professor (Research), Head of Research Translation and Mentorship
and of The Genital Microbiota and Mycoplasma Group Melbourne
School of Translational Medicine, Monash University and Alfred Hospital
Principal Research Fellow at the Burnet Institute
MedicalResearch.com: What is the background for this study?
Response: One in three women globally have bacterial vaginosis (BV), a condition that causes a malodourous discharge, and associated with serious gynaecologic and obstetric sequelae (including miscarriage and preterm birth) and increases the risk sexually transmitted infections (STIs) and HIV. Women with symptoms are treated with broad-spectrum antibiotics, however, over 50% of women experience BV recurrence within 3-6 months. The recurrence rate is even higher at 60-80% among women with an ongoing regular partner. Current practice is to simply retreat women experiencing BV recurrence with the same antibiotics, which leaves them (and clinicians) frustrated and distressed.
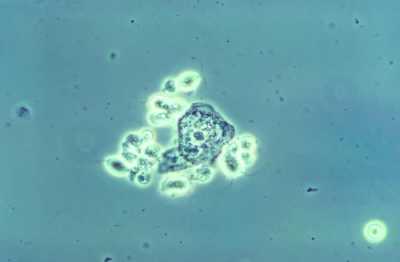
We and others have accumulated a body of evidence to show that BV has the profile of an STI. BV-associated bacteria are detected in men in the distal urethra and on penile-skin, and couples share these organisms. However, to date, has not been recommended for BV as it is for other STIs. This is largely because men do not usually have any symptoms, and past partner-treatment trials in the 1980s and 1990s, which only used oral antibiotics for men, failed to prevent BV recurrence, which was taken as conclusive evidence against sexual transmission. Reviews of these trials have since identified their limitations.
Given the evidence of male carriage of BV-associated bacteria at two genital sites, we hypothesised that both sites needed to be targeted with antimicrobial therapy to prevent re-infection post-treatment. The aim of our study was to assess if male partner-treatment concurrently with female treatment using a combination of oral and topical antibiotics for the first time, would decrease BV recurrence over 12 weeks compared to the current standard practice of treating women only.
(more…)







 Sean M Hughes MA
Department of Obstetrics and Gynecology
University of Washington
Seattle, WA
MedicalResearch.com: What is the background for this study?
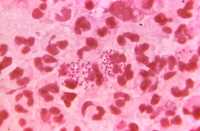
Response: Young women are at elevated risk of getting sexually transmitted infections at the age when they typically start to have sexual intercourse. It’s not known whether this elevated risk is a consequence of behavioral factors (such as choices around use of barrier protection), physiological factors (such as a difference in the immune system) or a combination of both. In this study, we investigated a physiological factor: the immune system in the vagina.
Sean M Hughes MA
Department of Obstetrics and Gynecology
University of Washington
Seattle, WA
MedicalResearch.com: What is the background for this study?
Response: Young women are at elevated risk of getting sexually transmitted infections at the age when they typically start to have sexual intercourse. It’s not known whether this elevated risk is a consequence of behavioral factors (such as choices around use of barrier protection), physiological factors (such as a difference in the immune system) or a combination of both. In this study, we investigated a physiological factor: the immune system in the vagina.