Infections, Laboratories / 27.03.2025
Strep Test Results: What the Colors Mean
Editor's note: Please remember there are other causes of a sore throat besides Strep bacteria, some of which may be serious including Mono (mononucleosis), Haemophilus, Whooping cough and others. Please consult your health care provider for specific medical advice. Information in this post is for background education only and not to be construed as specific medical advice.
A sore throat can be annoying. But if it comes with fever and swollen glands, it might be strep throat. Rapid strep throat tests give you quick results. But those color changes on the test strip can be confusing. Many people don’t know what they mean. Understanding these results is essential to knowing whether you are suffering from a viral infection or a strep throat. This guide explains strep test colors, what they mean, and what to do next.
How a Strep Throat Test Works
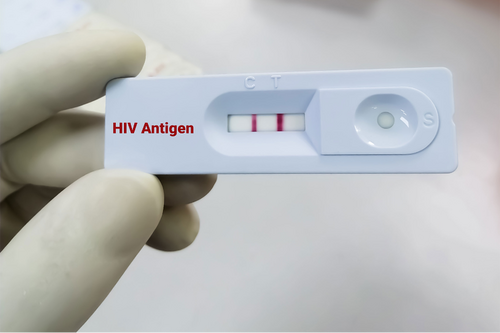
There are two main types of tests: the rapid antigen test and the throat culture.- Rapid antigen tests work by detecting proteins (antigens) from the strep bacteria using a chemical reaction .
- In the throat culture method, the sample is placed in a lab to grow bacteria if present.