Alzheimer's - Dementia, Author Interviews, Biomarkers / 11.12.2024
Novel Alzheimer’s Finding: Increasing Levels of Normal Protein, Aβ42 May Be Linked to Improvement
MedicalResearch.com Interview with:
Alberto J. Espay, MD, MSc, FAAN
Professor of Neurology
Director and Endowed Chair
Gardner Family Center for Parkinson's disease and Movement Disorders
University of Cincinnati Academic Health Center
MedicalResearch.com: What is the background for this study? What are the main findings
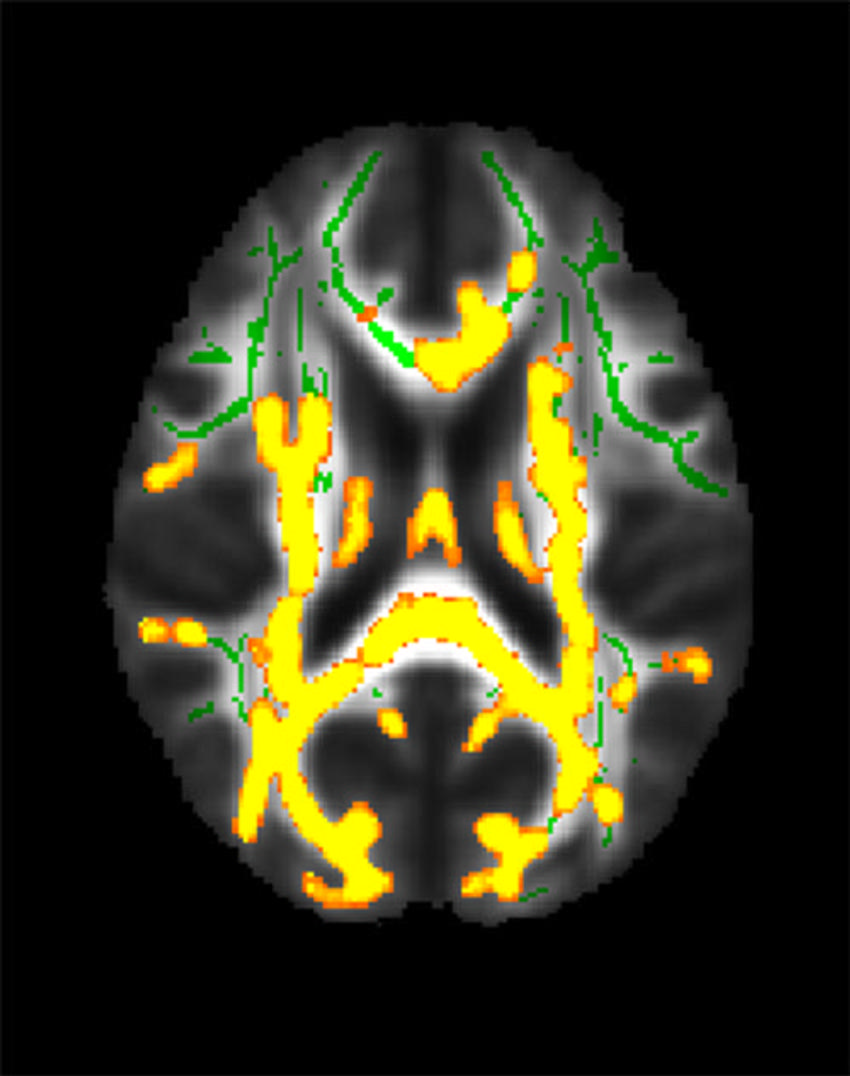
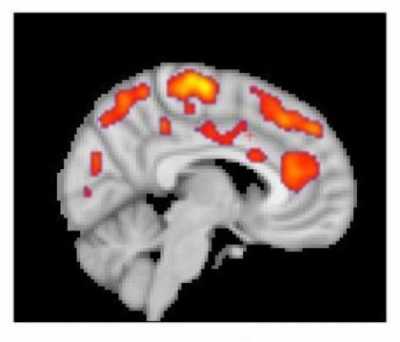
Response: Because aducanumab, lecanemab, and donanemab were only in a minority of anti-amyloid treatments showing a benefit, I was interested in finding out what makes them special. It turns out that they not only clean the brain from amyloid, like other monoclonal anti-Aβ antibodies, but they also increase Aβ42 in the spinal fluid, which is a measure of the normal protein in the brain. Everyone with Alzheimer’s has low Aβ42 levels because this protein clumps into amyloid plaques.
I tested the hypothesis that increasing Aβ42 could explain the cognitive outcomes at least as well as decreasing amyloid, and that’s exactly what we found. This suggests that restoring the normal protein levels, Aβ42, may explain why some anti-amyloid treatments (presumably those that increased those levels the most) come with benefits.
(more…)