Alzheimer's - Dementia, Author Interviews, Clots - Coagulation, Heart Disease / 23.11.2021
AHA21: GIRAF Study Results Comparing Anticoagulants and Cognitive Decline in AFib Patients
MedicalResearch.com Interview with:
Bruno Caramelli MD PhD
Associate Professor of Medicine
University of Sao Paulo, Brasil
Director, Interdisciplinary Medicine in Cardiology Unit
Chairman of the PhD program in Medical Sciences at the University of Sao Paulo, Brazil.
President of the Department of Clinical Cardiology at the Brazilian Society of Cardiology
FESC: Fellow of the European Society of Cardiology
MedicalResearch.com: What is the background for this study?
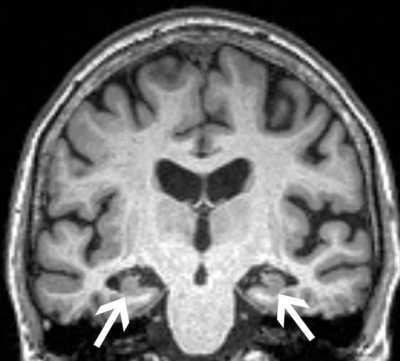
Response: Atrial fibrillation is the most common cardiac arrhythmia in older adults, and it is associated with an increased risk of stroke, cognitive impairment, and dementia. Stroke can occur when a blood clot blocks blood flow to the brain, and oral anticoagulants, such as dabigatran and warfarin, are typically prescribed to prevent stroke. Dabigatran has been found to be comparable to warfarin for the prevention of stroke and also has a lower risk of major bleeding complications.
Previous research has shown that people with atrial fibrillation taking oral anticoagulation therapy have a lower risk of dementia, however, the mechanism involved in this benefit is unknown, and previous clinical trials have not evaluated cognitive and functional impairment outcomes among patients.
It’s possible that cognitive decline is related to the formation of small blood clots in the brain, which is treated by effective medications that prevent blood clots. Since dabigatran offers a more stable anticoagulation status, we investigated whether it would be more effective than warfarin for the prevention of cognitive decline in patients with atrial fibrillation.
Previous studies were retrospective and observational studies and considered tests that evaluate global cognitive function in a generic, global, and non-specific way. In that way its not possible to exclude different causes of dementia as Alzheimer's disease and others making it difficult to establish an effect directly related to atrial fibrillation or the anticoagulation treatment.
(more…)