Author Interviews, Autism, Brigham & Women's - Harvard, Genetic Research / 26.08.2024
Autism: Study Sheds Light on Genetic Variants and Neurodevelopment Mechanisms
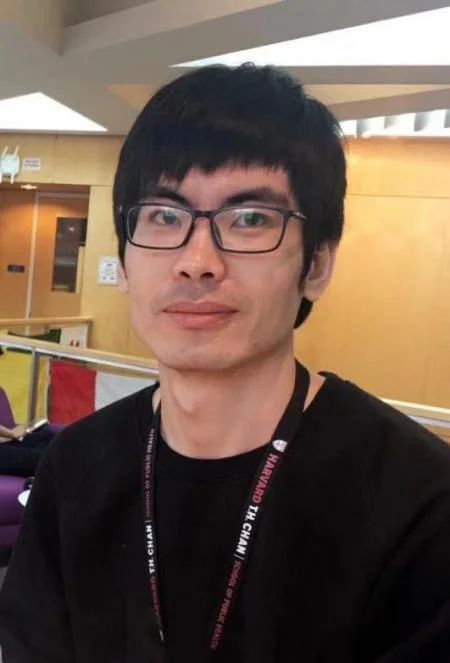
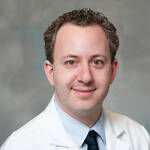
MedicalResearch.com Interview with:
Caroline Dias, M.D., Ph.D.
Assistant Professor, Pediatrics-Developmental Pediatrics
University of Colorado Anschutz Medical Campus
Christopher Walsh, M.D., Ph.D.
Chief, Division of Genetics and Genomics
Bullard Professor of Pediatrics and Neurology at Harvard Medical School
and researcher who has used material donated to the brain bank
MedicalResearch.com: What is the background for this study?
Response: Many different types of genetic variants contribute to neurodevelopmental disorders such as autism. Copy number variants are large pieces of genetic material that are duplicated or deleted. We have known for many years that many copy number variants at certain genetic locations are linked to autism. Because these copy number variants may include lots of different genes, it has been difficult to understand how these copy number variants alter human brain function. Furthermore, although animal models are important, autism is in many ways defined by differences in uniquely human cognitive and social functioning. Better understanding of how these copy number variants change human brain function will shed light on universal mechanisms that regulate neurodevelopment. We studied a copy number variant called dup15q, that is associated with almost 40-fold higher rates of autism vs. the general population. We studied post-mortem human brain tissue from individuals with dup15q, individuals with autism not related to dup15q, and neurotypical controls, to better understand how the human brain is impacted by dup15q. We focused on frontal cortex, an important brain region in executive function and social perspective taking. We applied cutting edge techniques that allow us to assess individual cells in the brain. (more…)