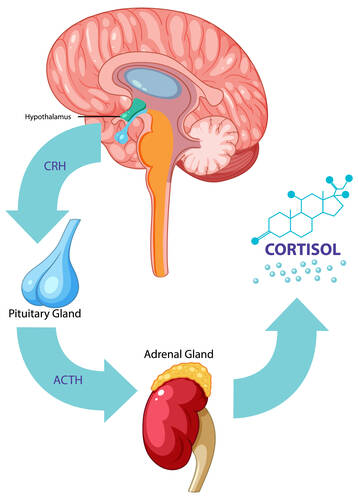
The endocrine system is a network of glands that produce and release hormones. These hormones control many vital body functions, including metabolism, growth, and reproduction. As we age, the efficiency of this system declines, leading to various age-related diseases and conditions. Understanding how the endocrine system impacts longevity can help us develop strategies to live longer and healthier lives.
Testosterone / 07.12.2024
What Does Free Testosterone Do? Understanding the Role of This Crucial Hormone
Editor's note: There are short and long term risks of TRT, including but not limited to liver, heart, blood and edema side effects. Testosterone Replacement Therapy (TRT) should be taken only under the direction of an experienced medical provider.
Testosterone, a key hormone found in both men and women (though typically in higher levels in men), contributes to that sense of drive and well-being. Many people know testosterone for its role in muscle mass, sexual health, and mood regulation. But did you know that not all testosterone is created equal? One important aspect of this hormone is what experts call “free testosterone.” While total testosterone measures all the hormone in your body, free testosterone focuses on the portion that’s ready to act. Understanding what free testosterone does can help you gain insights into your overall health and wellness. This post will dive into what free testosterone is, why it matters, the signs of low levels, and how you might naturally support healthier hormone balance. Let’s explore the science behind this powerful hormone in a friendly, easy-to-follow way.
Defining Testosterone and Its Forms
Testosterone is an androgen hormone, often associated with men’s health, but it plays roles in women’s bodies as well. In men, most testosterone is produced in the testes; in women, it’s produced in smaller amounts by the ovaries and adrenal glands. Testosterone influences a wide range of bodily functions, including muscle growth, bone density, mood stability, libido, and even aspects of cognitive function. However, not all testosterone found in the bloodstream is available for immediate use. When you see a “total testosterone” reading on a lab test, this number includes every bit of testosterone in the bloodstream. Most of it (around 98%) is bound to proteins such as sex hormone-binding globulin (SHBG) and albumin. Bound testosterone is essentially “parked” and not ready to jump into action. Free testosterone, on the other hand, makes up a much smaller percentage of the total, but it’s the portion that can easily interact with cells and do its job. Understanding this distinction can help you interpret lab results more meaningfully and offer clues about your energy, drive, and overall vitality. (more…)
Editor's note: This piece discusses suicide. If you have experienced suicidal thoughts or have lost someone to suicide and want to seek help, you can contact the Crisis Text Line by texting "START" to 741-741 or call the Suicide Prevention Lifeline at 800-273-8255.
Men's health has been getting more attention, thanks to advanced technology and new insights into male health problems. From hormone issues to mental health problems, men face unique struggles that need strategic solutions.
These days, treatments evolve rapidly, allowing men to feel better and live healthier lives. So, in honor of Men's Health Awareness Month, let's take a look at some of the latest treatments changing men's health.
Maintaining Healthy Testosterone Levels
Testosterone replacement therapy (TRT) supports men with low testosterone, also called hypogonadism. Low testosterone levels can lead to fatigue, low sex drive, mood swings, and muscle loss. TRT helps boost testosterone through injections, gels, patches, or pellets. TRT can make a major impact, bringing more energy, sharper focus, and renewed vitality. However, it must be done under medical care. Misuse can cause serious issues, like heart problems or an overload of red blood cells. Thus, finding a local clinic that specializes in TRT is key. For example, if you're in Seattle, seek a Seattle men's health clinic that specializes in such care. With proper guidance and routine checks, TRT can renew both body and mind. (more…)
Endocrinology, Hormone Therapy, Testosterone / 15.11.2024
Boost Your Immunity This Flu Season with These Proven Strategies
BHRT uses hormones that are biologically identical to those your body naturally produces. BHRT hormones are not FDA tested or...
Hormone Therapy, Legal-Malpractice / 02.11.2024
How to Seek Compensation for Harmful Effects of Depo-Provera
Depo-Provera, a famous contraceptive shot administered every three months, has been widely used to prevent pregnancy. While effective for many, Depo-Provera has been linked to severe side effects, including bone density loss, blood clots, and even brain tumors in rare cases. If you've experienced harmful effects from Depo-Provera, you may be qualified for a settlement for medical expenses, pain, suffering, and other damages. This guide outlines the steps and critical information to understand if you’re seeking compensation.
(more…)
Fertility, Hormone Therapy, Sexual Health / 01.11.2024
Understanding Birth Control Side Effects: What to Expect and How to Manage Them
Birth control or medical contraception is used for a variety of reasons, but its main role is to prevent unwanted pregnancies. There are many different types of birth control, so their function and ingredients vary. In general, they usually affect your hormones to make you unable to conceive 99% of the time. Birth control is also used to regulate hormonal imbalances, stop menstruation, or alleviate symptoms of conditions like polycystic ovarian syndrome (PCOS). Like any medication, birth control can come with some side effects, which may be mild for some and extreme for others. You and your doctor will factor in your health, medical history, potential side effects, and reproductive goals to figure out which birth control method is the best for your needs and body. When prescribed birth control, it’s important to understand common and uncommon side effects to avoid concerns and complications.
(more…)
Editor's note: This article discusses growth hormone for research purposes only. Do no take growth hormone or endocrine supplements unless specifically directed to do so by your health care provider.
Peptides have gained increasing interest in scientific domains due to their potential to regulate various biological processes. Growth Hormone-Releasing Peptide-2 (GHRP-2) and CJC-1295 have been of particular focus. While individually studied for their potential to modulate growth hormone release and other physiological functions, their combined implications for emerging research remain an emerging topic of interest.
This article aims to explore the potential implications of a GHRP-2 and CJC-1295 blend in scientific research, particularly in fields such as metabolism, tissue regeneration, and neurological function. The blend, by engaging with endocrine and cellular pathways, may open new research avenues in understanding and manipulating growth hormone (GH) signaling, tissue repair, and metabolic integrity.
(more…)
Hormone Therapy, Menopause / 04.10.2024
How Hormone Therapy Can Help Manage Symptoms and Improve Quality of Life
Hormone replacement therapy (HRT) has long been used to manage the disruptive symptoms associated with hormonal imbalances, particularly those caused by menopause in women and low testosterone in men. As the body ages, hormone levels naturally fluctuate, often leading to uncomfortable symptoms that can negatively impact one’s quality of life. HRT offers a solution by replenishing key hormones, providing relief from symptoms such as hot flashes, mood swings, and low energy.
Hormone replacement therapy involves supplementing the body with hormones that it no longer produces in adequate quantities. For women, this typically means replacing estrogen and progesterone, the hormones that regulate many aspects of the female reproductive system. For men, HRT usually focuses on replenishing testosterone, which naturally declines with age.
While the primary goal of HRT is to relieve symptoms, it can also improve long-term health. Estrogen, for example, helps protect against bone loss, and testosterone replacement in men can prevent muscle atrophy. But before diving into the benefits of HRT, it's important to understand why hormone levels fluctuate and how these changes affect the body.
(more…)
Endocrinology, Hormone Therapy / 02.10.2024
The Physiological Research Behind Growth Hormone Releasing Hormone (GHRH)
Studies suggest that Growth Hormone-Releasing Hormone (GHRH) is a peptide with profound implications for the regulation of growth and metabolic processes. This article delves into the intricate roles of GHRH, exploring its functions, potential impacts, and the complex physiological mechanisms influenced by this peptide.
Overview of Growth Hormone-Releasing Hormone
Growth Hormone-Releasing Hormone (GHRH) is a peptide consisting of 44 amino acids. It is primarily synthesized and secreted by the arcuate nucleus of the hypothalamus. The principal function of GHRH is believed to be to stimulate the anterior pituitary gland to release Growth Hormone (GH). This cascade is considered to play a crucial role in regulating various physiological functions, including growth, metabolism, and tissue repair.
Studies suggest that GHRH may act on the pituitary gland by binding to specific GHRH receptors located on pituitary somatotroph cells. These receptors are G protein-coupled receptors (GPCRs) that may activate intracellular signalling pathways, ultimately leading to the secretion of GH. GH, in turn, is believed to impact numerous tissues and organs, further influencing a wide array of physiological processes.
(more…)
Endocrinology, Pharmacology / 20.09.2024
The Science and Benefits Behind Next-Generation Hormone Regulation Treatments
Editor's note: Consult with your medical provider beginner any form of potential hormonal regulation therapy.
The discussion below has not been FDA verified or approved and should not be construed as specific medical advice.
The field of hormone regulation has evolved significantly, offering new treatments that aim to restore balance and improve overall well-being.
MedicalNewsToday states that most people go through natural hormonal fluctuations at various stages of their lives. However, imbalances can emerge when the endocrine glands, which create and release hormones into the circulation, do not operate properly. These glands are distributed throughout the body, and each of them handles different organs and physical activities.
As more individuals seek solutions for hormone-related issues like fatigue, weight gain, and mood swings, next-generation hormone regulation treatments are becoming increasingly popular.
These innovative therapies, such as hormone pellet therapy, bioidentical hormone replacement therapy (BHRT), and peptide therapy, target specific imbalances to provide personalized solutions. These treatments offer hope for improved health, vitality, and quality of life by addressing the root causes of hormone disruptions.
(more…)
It is important to work closely with a doctor to monitor your treatment and adjust it if needed. Not all...
Endocrinology, Supplements, Thyroid Disease / 17.07.2024
Thyroid Health: Should you take Thyroid-Specific supplements?
Find out if thyroid-specific supplements are right for you, the benefits, and the risks....
Endocrinology, Exercise - Fitness, Genetic Research / 21.05.2024
Health and Wellness – 6 New Trends Offering Benefits for the Masses
As public interest in health and wellness continues to grow, so does the number of innovative trends aimed at improving physical, mental, and emotional well-being. These new trends offer accessible and effective ways to enhance lifestyle choices and promote overall health. Individuals need to stay informed about these developments to make educated decisions that align with their health goals. By embracing novel and scientifically backed wellness practices, people can significantly enhance their quality of life, finding balance and improved health through modern solutions.
1. Digital Fitness Apps
Digital fitness apps have redefined the way people engage with personal fitness, providing tools that help users manage their health and wellness directly from their smartphones. These apps offer a range of functionalities, including personalized workout plans, step tracking, calorie counting, and even virtual coaching sessions. The integration of these features makes it easier for users to stay committed to their fitness goals, providing a convenient and adaptable approach to exercise that fits into the user's lifestyle. The benefits of digital fitness apps extend beyond simple workout assistance; they also play a crucial role in motivating users to stay active and healthy. By setting personalized goals and receiving instant feedback on progress, users can see tangible results that encourage continued effort. Additionally, many apps now offer social connectivity features, allowing users to join communities of like-minded individuals who support and inspire each other. This sense of community can be particularly motivating, making it easier for individuals to maintain a consistent fitness routine. (more…)
Author Interviews, Depression, Endocrinology, Nature / 27.08.2023
USC Study Finds Strong Correlation Between Estrogen-Reactive Hormones and Depressive States
MedicalResearch.com Interview with:
Huizhong Whit Tao, PhD
Professor of Physiology & Neuroscience
Zilkha Neurogenetic Institute
Department of Physiology & Neurosience
Keck School of Medicine
University of Southern California
MedicalResearch.com: What is the background for this study?
Response: Previously, we published a study in which we found that a group of neurons, namely glutamatergic neurons, in the medial preoptic area (MPOA) of the hypothalamus mediate stress-induced anxiety states. This result inspired us to explore whether the MPOA can play a more general role in mood regulation. Fluctuations in the productive hormones secreted by women’s ovaries are known to cause mood swings.
In some cases, rapid changes in the secretion of ovarian hormones can cause depressive-like symptoms. Key examples are postpartum and peri-menopausal depression. In this study, we intended to test whether the MPOA can also play a part in depressive states that are linked to fluctuations in ovarian hormones.
(more…)
Author Interviews, Brigham & Women's - Harvard, Endocrinology, Fertility, Lancet, OBGYNE / 25.07.2023
Early Brigham Study Uses Stem Cells To Restore Ovarian Function
MedicalResearch.com Interview with:
Raymond M. Anchan, MD, Ph.D.
Director, Stem Cell Biology and Regenerative Medicine Research Laboratory
Assistant Professor, Harvard Medical School
Obstetrics/Gynecology
Center for Infertility and Reproductive Surgery
Brigham and Women's Hospital
MedicalResearch.com: What is the background for this study?
Response: As a reproductive endocrinologist, I have the privilege of caring for patients who unfortunately experience premature ovarian insufficiency- Some of these patients are as young as 17 yo. Additionally, a significant number of patients over the years have been reproductive age women who have breast cancer and ovarian failure from chemotherapy. These patients have been my inspiration to try to find a treatment for them. Since my earlier days as a neurobiologist and stem cell scientist, it was a natural course for me to seek cell-based therapies that are patient specific using autologous iPSCs.
(more…)
Author Interviews, Endocrinology, Hormone Therapy, Menopause / 17.07.2023
Study Evaluates Progesterone Therapy for Perimenopausal Night Sweats and Hot Flushes
MedicalResearch.com Interview with:
Jerilynn C Prior MD FRCPC (on behalf of all authors
Professor of Endocrinology / Department of Medicine
University of British Columbia
Centre for Menstrual Cycle and Ovulation Research www.cemcor.ca
BC Women’s Health Research Institute
Vancouver BC Canada
MedicalResearch.com: What is the background for this study?
Response: Night sweats and hot flushes/flashes (together called vasomotor symptoms, VMS) disturb women who are still menstruating (in perimenopause) are at least as much or more than menopausal women (without flow for a year or more)1. However, although studies have investigated various treatments for perimenopausal hot flushes/flashes, none have proven effective in these women who are also likely to be having heavy flow, breast tenderness, and premenstrual symptoms related to high and variable estrogen levels. These include randomized controlled trials (RCT) of the birth control pill2, and gel estrogen in women using a progestin-releasing IUD3.
Neither showed that therapy was more effective than placebo; both studied too few participants to provide a clear answer.
Meanwhile, major medical organization guidelines recommend menopausal hormone therapy (MHT, usually of estrogen with a progestin) for any women younger than 60 years old who are bothered by night sweats and hot flushes 4-6. However, there are no scientific RCT studies showing MHT is effective for perimenopausal night sweats and hot flushes. Giving more estrogen to someone whose own estrogen levels are often high, also did not make clinical sense.
We previously performed an RCT showing that oral micronized progesterone (progesterone) was effective for menopausal hot flushes and also improved sleep7. Given that progesterone levels in perimenopausal women are declining, we considered that perimenopausal progesterone therapy for night sweats needed testing.
(more…)
Author Interviews, Biomarkers, Brigham & Women's - Harvard, Diabetes, Endocrinology / 26.06.2023
ENDO23: Study Correlates Dietary Sugar End Products with Skin Autofluorescence Findings
MedicalResearch.com Interview with:
Dr. Bita Zahedi MD MA
Endocrinologist
Massachusetts General Hospital
MedicalResearch.com: What is the background for this study?
Response: The purpose of this study was to develop and validate a measure of dietary advanced glycation end-products (AGEs) to investigate the role of dietary AGEs in diabetic disease processes. AGEs are a group of highly reactive compounds involved in the pathophysiology of diabetic complications, such as microvascular disease, cardiomyopathy, and possibly bone health. AGEs form through a nonenzymatic reaction between reducing sugars and free amino groups of proteins, lipids, and nucleic acids, also known as a Maillard or browning reaction.
Endogenous AGE formation and accumulation is a normal part of metabolism and aging, however the process of glycation can be enhanced by hyperglycemia, hyperlipidemia, and increased oxidative stress. Additionally, AGEs can be absorbed from exogenous sources via consumption of various food items. Prior studies demonstrate that skin AGEs are predictive of Dietary AGEs (dAGEs) which are naturally present in certain uncooked foods, mainly animal-derived products, furthermore the method of food preparation can result in significant AGE formation. Considering the ubiquitous intake of dAGEs, it is possible that the consumption of exogenous AGEs contribute to AGE-induced oxidative stress, inflammation, and its subsequent detrimental sequalae.
(more…)
Author Interviews, Endocrinology, Gender Differences, Weight Research / 16.06.2023
ENDO2023: Mass General Study Identifies Sex Differences in Neurohormone Linked to Body Composition
MedicalResearch.com Interview with:
Francesca Galbiati, MD
Clinical/Research fellow in Endocrinology
Massachusetts General Hospital
MedicalResearch.com: What is the background for this study?
Response: Arginine-vasopressin (AVP) is a neurohormone well known for its role in water balance regulation. It promotes renal water absorption in the kidney, to maintain normal sodium levels in the blood via a tightly controlled osmotic regulation. Besides AVP classical role, data have shown that AVP effects extend beyond water balance regulation. Animal studies have shown that AVP has metabolic effects, including reducing food intake, inducing lipolysis, and promoting muscle regeneration in male mice.
Furthermore, AVP is regulated differently in males and females, and affects cognition differently across sexes, a phenomenon called sexual dimorphism. However, it is unknown whether its dimorphism translates to metabolism. Also, findings on AVP metabolic role are inconsistent, possibly due to the opposing effects of AVP at different receptor subtypes, which regulation is still largely unknown. We performed this study to better investigate AVP metabolic role, and explore sex differences. We hypothesized that AVP would be positively associated with BMI, adiposity, and lean mass (acting as a signal of energy availability). We also predicted that relationships between AVP and body composition measures would differ by sex. We used the AVP area under the curve around a standardized meal to better capture repeated measures in response to food intake (that directly impacts energy availability). This also allowed to avoid the possible risk of fluctuating AVP levels due to possible pulsatile secretion.
(more…)
Author Interviews, Endocrinology, Environmental Risks / 23.02.2023
Ubiquitous Environmental Hormone Disrupter Linked to Broad Range of Diseases
MedicalResearch.com Interview with:
Jesse Goodrich PhD
Assistant Professor
Department of Population and Public Health Sciences
Keck School of Medicine
University of Southern California
MedicalResearch.com: What is the background for this study?
Response: Per- and poly-fluoroalkyl substances (PFAS) are a group of persistent chemicals that are known to interfere with hormones and metabolism. In our previous research, we have found that PFAS exposure is associated several specific diseases, especially in children and adolescents. These include obesity, type 2 diabetes, liver disease, and even liver cancer. However, we are still only just starting to fully understand all of the health effects of the many different PFAS in existence. Previous studies have focused primarily on one or two main PFAS. However, there are over 9,000 known PFAS, and people are exposed not just to a single PFAS but to mixtures of many PFAS. Importantly, the combination of these chemical exposures may affect us differently than single exposures alone.
To address this challenge, we used an innovative approach to study design to examine how exposure to PFAS impacts biological processes which may underly the development of many different diseases in adolescents and young adults. To do this, we first measured thousands of naturally occurring chemicals, known as metabolites, in people's blood. Then, using a new biostatistical method developed by our team, we identified how exposure to a mixture of several PFAS impacted each individual chemical. Finally, we used this information to determine which biological processes are changed by PFAS exposure.
(more…)
Author Interviews, Endocrinology, Heart Disease, Kidney Stones / 10.08.2022
Increased Adrenal Hormone Aldosterone Linked to Greater Risk of Chronic Kidney Disease
MedicalResearch.com Interview with:
Ashish Verma, MD
Assistant Professor, Nephrology
Department of Medicine
Boston University
MedicalResearch.com: What is the background for this study? Would you tell us a little about aldosterone?
Response: “Recent randomized, controlled trials have shown that a drug called finerenone is effective in delaying CKD progression and adverse cardiovascular outcomes in patients with chronic kidney disease and diabetes. However, the role of aldosterone in this process was not directly investigated and levels of the hormone were not measured,”
“Since excessive levels of aldosterone is common, yet mostly unrecognized, we hypothesized that one reason why finerenone was effective in lowering the risk of CKD progression was that it was treating unrecognized high concentrations of the hormone.”
To study this we investigated the associations between aldosterone concentrations in the blood and kidney disease progression among 3680 participants in the Chronic Renal Insufficiency Cohort study, which ran in seven clinics in the US between 2003 and 2008. The participants were aged between 21 and 74 years old.
Aldosterone is a steroid hormone secreted by the adrenal glands, which sit above the kidneys. Its main role is to regulate salt and water in the body, and so it plays a central role in controlling blood pressure. Too much of it can lead to high blood pressure, cardiovascular and kidney diseases.
(more…)
Author Interviews, Brigham & Women's - Harvard, Endocrinology, Hip Fractures, NEJM, Osteoporosis, Vitamin D / 27.07.2022
Brigham Study of Supplemental Vitamin D and Risk of Bone Fractures Reported in NEJM
MedicalResearch.com Interview with:
Meryl S. LeBoff, MD
Chief, Calcium and Bone SectionDirector of the Skeletal Health and Osteoporosis CenterDirector, Bone Density UnitDistinguished Chair in Skeletal Health and Osteoporosis
Professor of Medicine, Harvard Medical School
Endocrinology, Diabetes and Hypertension, Women's Health
Brigham And Women's Hospital
JoAnn E. Manson, MD, DrPH
Professor, Epidemiology, Harvard T.H. Chan School Of Public Health
Michael and Lee Bell Professor of Women's Health, Medicine, Harvard Medical School
Chief, Preventive Medicine, Brigham And Women's Hospital
Co-Director, Womens Health, Brigham And Women's Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Osteoporosis is a major public health problem. Although supplemental vitamin D has been widely used to reduce the risk of fractures in the general population, studies of the effects of vitamin D on fractures, the most important bone health outcome, have been conflicting.
Randomized controlled trials, the highest quality studies, from around the world have shown benefit, no effect, or even harm of supplemental vitamin D on risk of fractures. Some of the trials used bolus dosing, had small samples sizes or short study duration, and co-administered calcium. No large RCTS of this scale tested whether daily supplemental vitamin D (without co-administration with calcium) prevented fractures in the US population.
To fill these knowledge gaps, we tested the hypothesis in this ancillary study to VITAL, whether daily supplemental vitamin D3 reduced the risk of incident total, non-spine and hip fractures in women and men in the US.
(more…)
Author Interviews, Endocrinology, Nutrition, Testosterone, Weight Research / 11.03.2022
Links Between Diet and Men’s Testosterone Levels
MedicalResearch.com Interview with:
Joe Whittaker, MSc
Nutritionist
MedicalResearch.com: What is the background for this study?
Response: There are several studies showing a generational decline in men's testosterone levels, beginning in the 1970s. This is due to a variety of factors such as poorer diets, lack of physical activity, and increasing toxin exposure. Therefore, there is intense research interest in ways we can optimise testosterone levels, to combat this generational decline.
Some well-known studies have found low-carbohydrate diets boost testosterone levels, but others have show the reverse effect. So, to settle the controversy we gathered and reanalysed all known studies on the topic. There was also the question of high protein diets and their effects on testosterone, which are currently disputed.
(more…)
Author Interviews, Brigham & Women's - Harvard, Endocrinology, Insomnia, Menopause, Sleep Disorders, Weight Research / 23.03.2021
Poor Sleep During Menopause Linked to Decreased Fat Metabolism
MedicalResearch.com Interview with:
Leilah K. Grant, PhD
Postdoctoral Research Fellow in Medicine
Brigham and Women’s Hospital
Harvard Medical School
MedicalResearch.com: What is the background for this study?
Response: The prevalence of obesity increases in women around the age of menopause which increases the risk of diseases like diabetes and heart disease. Changes in hormones, like estrogen, are thought to contribute to weight gain during menopause, but other common symptoms of menopause such as sleep interruption may also play a role. While short sleep is known to adversely affect metabolism, little is known about the metabolic consequences of the type of sleep disruption most common in menopausal women – increased nighttime awakenings (i.e., sleep interruption) caused by hot flashes, but no change in overall sleep duration. We therefore did this study to see how an experimental model menopause-related sleep interruption would affect metabolic outcomes that may contribute to weight gain. (more…)
Author Interviews, Endocrinology, Heart Disease, Women's Heart Health / 05.08.2020
Higher Risk of Cardiovascular Disease in Women with PCOS
MedicalResearch.com Interview with:
Dr. Clare Oliver-Williams PhD
University of Cambridge
MedicalResearch.com: What is the background for this study?
Response: Women with PCOS are known to be at greater risk of CVD, however the some symptoms (menstrual irregularity) of PCOS are specific to reproductive age women. This raises the question of whether CVD risk varies across by age, which was the focus of my research with colleagues at the University of Copenhagen.
MedicalResearch.com: What should readers take away from your report?
Response: Women with PCOS were at 19% higher CVD risk than women without CVD, however once the association was stratified by age, there was no evidence for a higher CVD risk for women older than 50.
(more…)
Author Interviews, Endocrinology, Thyroid Disease / 11.06.2020
Thyroid Eye Disease Can Have Long Term Impact on Vision, Eye Appearance and Quality of Life
MedicalResearch.com Interview with:
 Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
 Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
Elizabeth H.Z. Thompson, Ph.D.
Group vice president, Clinical Development and External Search
Horizon Therapeutics
MedicalResearch.com: What is the background for this study?
Response: This study provides the first U.S.-based validation of the Graves' Ophthalmopathy Quality of Life (GO-QOL) questionnaire. For your background, Graves’ Ophthalmopathy is another term used to describe Thyroid Eye Disease (TED). The GO-QOL questionnaire includes eight questions, each on visual functioning and appearance-related impacts of TED on patients. Though widely used and validated in Europe, the relevance of the questions for patients in the United States hasn’t previously been explored.For this evaluation, 13 eligible TED patients completed the questionnaire and then underwent a separate cognitive QOL-related interview. (more…)
Author Interviews, Endocrinology, Environmental Risks, JCEM, Menopause / 05.06.2020
“Forever Chemicals” Linked To Earlier Onset of Menopause
MedicalResearch.com Interview with:
Ning Ding MPH, PhD candidate
Sung Kyun Park Sc.D, MPH
Associate Professor
Department of Epidemiology
University of Michigan School of Public Health
Ann Arbor, MI 48109
MedicalResearch.com: What is the background for this study?
Response: Per- and polyfluoroalkyl substances (PFAS), also known as ‘forever chemicals’, are a family of synthetic chemicals used in a wide variety of nonstick and waterproof products and firefighting foams. The main issue is that PFAS are everywhere. It has been estimated that 110 million Americans, 1 out of three, may consume drinking water contaminated with PFAS. PFAS are very persistent and once PFAS enter the body, they don't break down and build up in the body over time.
(more…)
Author Interviews, CMAJ, Endocrinology, OBGYNE / 02.06.2020
Are Too Many Pregnant Women Being Diagnosed and Treated for Thyroid Disease?
MedicalResearch.com Interview with:
Lois Donovan MD FRCPC
Clinical Professor
Cumming School of Medicine
Division on Endocrinology and Metabolism and
Department of Obstetrics and Gynecology
University of Calgary
MedicalResearch.com: What is the background for this study?
1) We observed in our clinical practices that minor TSH elevations in early pregnancy frequently normalized without intervention.
2) Recent randomized control trials have failed to show benefit of treating women with levothyroxine with minor TSH elevations in pregnancy (more…)
Author Interviews, Endocrinology, Weight Research / 04.05.2020
People With More Brown Fat May Burn Fuel More Efficiently
MedicalResearch.com Interview with:
Florian Keifer, M.D., Ph.D
Associate Professor of Medicine
Division of Endocrinology and Metabolism
Department of Medicine III
Medical University of Vienna
MedicalResearch.com: What is the background for this study?
Response: Brown fat, in contrast to white fat, burns significant amounts of chemical energy through heat production. In numerous animal models the activation of brown adipose tissue (BAT) increases energy expenditure and counteracts weight gain. Therefore BAT has been established as a promising target in the fight against obesity and related metabolic disorders. In humans, BAT can be activated by moderate cold exposure, however the function and relevance of BAT are incompletely understood. Using PET scans we identified two groups of individuals those with and without active BAT and studied their differences in energy expenditure and blood fatty acid composition. (more…)
Author Interviews, Endocrinology, OBGYNE / 14.04.2020
PCOS: Regular Yoga May Decrease Testosterone Levels
MedicalResearch.com Interview with:
 Diana Speelman, Ph.D.
Director of Research for the College of Medicine
Associate Professor of Biochemistry
Reproductive System Course Coordinator
L|E|C|O|M
Erie, PA 16509
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by PCOS?
Response: Polycystic ovary syndrome (PCOS) is the most common hormone disorder in women of reproductive age. It is characterized by high androgen levels (e.g., testosterone) in the blood and irregular menstrual cycles. Despite affecting 5-15% of women, its cause is unknown. While medications can be used to reduce androgen levels, or help achieve menstrual regularity or stimulate ovulation, these often have undesirable side effects. Our goal was to investigate the effectiveness of non-pharmacologic approaches, including yoga, on improving the characteristics associated with the disorder. (more…)
Diana Speelman, Ph.D.
Director of Research for the College of Medicine
Associate Professor of Biochemistry
Reproductive System Course Coordinator
L|E|C|O|M
Erie, PA 16509
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by PCOS?
Response: Polycystic ovary syndrome (PCOS) is the most common hormone disorder in women of reproductive age. It is characterized by high androgen levels (e.g., testosterone) in the blood and irregular menstrual cycles. Despite affecting 5-15% of women, its cause is unknown. While medications can be used to reduce androgen levels, or help achieve menstrual regularity or stimulate ovulation, these often have undesirable side effects. Our goal was to investigate the effectiveness of non-pharmacologic approaches, including yoga, on improving the characteristics associated with the disorder. (more…)
 Diana Speelman, Ph.D.
Director of Research for the College of Medicine
Associate Professor of Biochemistry
Reproductive System Course Coordinator
L|E|C|O|M
Erie, PA 16509
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by PCOS?
Response: Polycystic ovary syndrome (PCOS) is the most common hormone disorder in women of reproductive age. It is characterized by high androgen levels (e.g., testosterone) in the blood and irregular menstrual cycles. Despite affecting 5-15% of women, its cause is unknown. While medications can be used to reduce androgen levels, or help achieve menstrual regularity or stimulate ovulation, these often have undesirable side effects. Our goal was to investigate the effectiveness of non-pharmacologic approaches, including yoga, on improving the characteristics associated with the disorder. (more…)
Diana Speelman, Ph.D.
Director of Research for the College of Medicine
Associate Professor of Biochemistry
Reproductive System Course Coordinator
L|E|C|O|M
Erie, PA 16509
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by PCOS?
Response: Polycystic ovary syndrome (PCOS) is the most common hormone disorder in women of reproductive age. It is characterized by high androgen levels (e.g., testosterone) in the blood and irregular menstrual cycles. Despite affecting 5-15% of women, its cause is unknown. While medications can be used to reduce androgen levels, or help achieve menstrual regularity or stimulate ovulation, these often have undesirable side effects. Our goal was to investigate the effectiveness of non-pharmacologic approaches, including yoga, on improving the characteristics associated with the disorder. (more…)
Author Interviews, Endocrinology, Ophthalmology, Thyroid Disease / 06.04.2020
Teprotumumab-Tepezza Reduces Proptosis in Patients with Thyroid Eye Disease
MedicalResearch.com Interview with:
Dr. Raymond Douglas MD PhD
Board Certified Oculoplastic Surgeon
Beverly Hills, CA
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by proptosis? How does teprotumumab work?
Response: This study provides pooled efficacy data from the Phase 2 and 3 clinical trials of teprotumumab showing that the recently FDA-approved medicine effectively reduces proptosis, also known as eye bulging, in patients with Thyroid Eye Disease (TED) regardless of age, gender and smoking status. Proptosis is one of the most debilitating symptoms of TED, especially given the accompanying pain, vision impairment and emotional distress.
Teprotumumab is a fully human monoclonal antibody and a targeted inhibitor of the IGF-1 receptor. In patients with Thyroid Eye Disease, the IGF-1 receptor is overexpressed on orbital tissues and when activated, causes inflammation and enlargement of ocular muscles, expansion of orbital tissue and fat and forward displacement of the eye, resulting in eye bulging. The proteins in teprotumumab target and bind to the IGF-1 receptor and inhibit its function, thereby reducing inflammation, preventing tissue expansion behind the eye, and preventing muscle and fat tissue remodeling. Based on this mechanism of action, it is believed that teprotumumab addresses the underlying biology of the disease. (more…)