MedicalResearch.com Interview with:
Vincent Guilamo-Ramos, PhD
MPH, LCSW, RN, ANP-BC, PMHNP-BC, AAHIVS, FAAN
Vincent Guilamo-Ramos is dean and professor at the Duke University School of Nursing, vice chancellor for nursing affairs, Duke University, and director of the Center for Latino Adolescent and Family Health (CLAFH) at Duke.
Dr. Guilamo-Ramos served as a member of the National Academies of Sciences, Engineering, and Medicine (National Academies) Committee on Prevention and Control of STIs in the U.S. that wrote the recent consensus study report. He also serves as a member of the Presidential Advisory Council on HIV/AIDS (PACHA) and the HHS Panel on Antiretroviral Guidelines for Adults and Adolescents.
MedicalResearch.com: What is the background for this study?
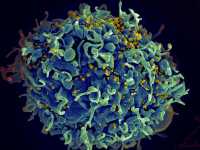
Response: The National Academies of Sciences, Engineering, and Medicine (National Academies) recently released a consensus study report on prevention and control of sexually transmitted infections (STIs) in the United States. The report entitled “Sexually Transmitted Infections: Adopting a Sexual Health Paradigm” includes a strong emphasis on adolescents and young adults as an important priority population for the response to record-level STI rates that have reached an all-time high for the sixth year in a row in 2019. The report also highlights the well-supported and crucial role of parents in addressing STIs and promoting sexual health among adolescents and young adults. In
this new Viewpoint article, my co-authors and I, who contributed to the National Academies report as committee members or consultants, discuss the practical implications for health care professionals of engaging parents in adolescent sexual health services.
(more…)