Addressing Pelvic Pain with the Intimate Rose Pelvic Wand
Survey Identifies Impact of Psychedelics on Sexual, Gender, and Intimate Relationships
Does evergreening contribute to the prescribing pattern of citalopram and escitalopram to U.S. Medicaid and Medicare patients?
Parita K. Ray
Medical Student
Department of Medical Education
Geisinger College of Health Sciences
Scranton, PA 18509
MedicalResearch.com: What is the background for this study?
- Citalopram and escitalopram are two of the most commonly prescribed antidepressants in the U.S. and are widely used for treating major depressive disorder (MDD) and generalized anxiety disorder (GAD), along with various off-label indications. While both medications share similar mechanisms of action, escitalopram was introduced as a purified version of citalopram’s active enantiomer. Despite little evidence showing a clear superiority of escitalopram over citalopram in efficacy or tolerability, prescribing trends appear to favor escitalopram, raising concerns about "evergreening"—a practice where pharmaceutical companies promote newer formulations of existing drugs to extend market exclusivity. Prior research has shown variations in the prescription rates of psychotropic medications across states and within specific populations, particularly among Medicaid and Medicare patients. However, little is known about the long-term prescribing patterns of citalopram versus escitalopram in these populations and whether these trends reflect potential evergreening practices.
The Benefits of Inpatient Rehab in Los Angeles for Addiction Recovery
A Distraction-Free Healing Environment
One of the biggest advantages of inpatient rehab in Los Angeles is the opportunity to step away from the triggers and stressors of daily life. At home, temptations, unhealthy relationships, or stressful work conditions can make recovery more challenging. In a dedicated rehab facility, you can fully focus on your healing without distractions. (more…)How to Make Informed Health Decisions for Better Well-Being
Understand Your Health Needs
Everyone’s health journey is different. Some people may be managing a chronic condition, while others want to stay on top of their general wellness. The first step in making informed decisions is to take time to understand your own health needs. That might include knowing your family history, keeping track of any symptoms you have, or noticing changes in your mood, energy, or physical health. When you are more aware of how you feel day to day, it becomes easier to spot when something needs attention. You should also think about your lifestyle. Do you get enough sleep? Are you eating balanced meals? Do you feel stressed all the time? These things all play a role in your overall health. (more…)Navigating Life After Addiction: Steps Towards Healing and Renewal
 Navigating life during this phase means adopting new habits, promoting a strong support system, and prioritizing mental and emotional well-being. This article will explore all the essential steps toward healing and recovery for those who have overcome the addiction challenge and are striving to build a fulfilling life.
Navigating life during this phase means adopting new habits, promoting a strong support system, and prioritizing mental and emotional well-being. This article will explore all the essential steps toward healing and recovery for those who have overcome the addiction challenge and are striving to build a fulfilling life.
Acknowledging the Journey Away from Drug Abuse
Are you going through drug addiction recovery? Taking a step back and recognizing how far you have come is essential. Drug or alcohol addiction is a struggle. To overcome it, intense efforts and dedication are required. By acknowledging your progress, you can build confidence and maintain motivation. It is important to celebrate milestones throughout your journey. Whether it is one month, six months, or one year of sobriety, they serve as reminders of personal growth and resilience. (more…)Study Finds Maternal Cannabis Use Associated with Behavior Disorders in Children
Luxury Rehab Clinic in St Helens
How to Deal with Hangover Anxiety: Effective Strategies and Tips
 Experiencing a hangover can be a challenging ordeal, not just physically but mentally as well. For many, the aftermath of a night of indulgence is accompanied by a wave of anxiety that can feel overwhelming. This phenomenon, often referred to as hangover anxiety, can exacerbate feelings of guilt, worry, and unease. Understanding how to manage these feelings is crucial for a smoother recovery. Below are effective strategies and tips to help navigate hangover anxiety.
Experiencing a hangover can be a challenging ordeal, not just physically but mentally as well. For many, the aftermath of a night of indulgence is accompanied by a wave of anxiety that can feel overwhelming. This phenomenon, often referred to as hangover anxiety, can exacerbate feelings of guilt, worry, and unease. Understanding how to manage these feelings is crucial for a smoother recovery. Below are effective strategies and tips to help navigate hangover anxiety.
Understanding Hangover Anxiety
Hangover anxiety is a specific type of anxiety that occurs after consuming alcohol. It often manifests as feelings of dread, worry about past actions, or fear of the future. This reaction is not uncommon, as alcohol can disrupt the balance of neurotransmitters in the brain, leading to heightened anxiety levels. Many individuals find themselves reflecting on the previous night's events, replaying conversations, and scrutinizing their behavior, which can exacerbate feelings of anxiety. (more…)Transforming Recovery: The Impact of Addiction Treatment Technology
 Research has shown that when technology-based interventions are designed using evidence-based behavioral and multimedia learning principles, they can significantly improve treatment outcomes. By offering new ways to assess, prevent, and treat addiction, these tools are enhancing traditional treatment programs and expanding the reach of recovery support systems.
Moreover, technology allows for more personalized care, enabling individuals to access resources and guidance whenever and wherever they need it. This article will explore how various technological advancements are improving addiction treatment and what the latest research reveals about their effectiveness.
Research has shown that when technology-based interventions are designed using evidence-based behavioral and multimedia learning principles, they can significantly improve treatment outcomes. By offering new ways to assess, prevent, and treat addiction, these tools are enhancing traditional treatment programs and expanding the reach of recovery support systems.
Moreover, technology allows for more personalized care, enabling individuals to access resources and guidance whenever and wherever they need it. This article will explore how various technological advancements are improving addiction treatment and what the latest research reveals about their effectiveness.
What Is Substance Use Treatment?
Substance use treatment refers to the comprehensive process of helping individuals recover from addiction to drugs, alcohol, or other harmful substances. This treatment aims to eliminate or reduce substance use, address the underlying causes of addiction, and equip individuals with the tools and skills needed to maintain long-term recovery. Effective substance use treatment is designed to improve overall well-being, including mental health, physical health, social relationships, and quality of life. (more…)Why Attending Support Groups More Frequently During Difficult Times Helps Manage the Stress
 Life in recovery can feel overwhelmingly difficult at times. We live in a stressful era and often don’t notice stress building up until it’s too late. The temptation to isolate can be hard to resist, and this allows many people to pursue their addiction in private. Support groups can be a key part of any successful relapse prevention effort.
Humans are social creatures, and addiction often takes away some of that humanity. It can fill the addicted person with shame and self-loathing. It can isolate people from their loved ones and keep them from doing things they enjoy.
In recovery, activities with other recovering people can be the glue that holds your new life together. Support groups—especially 12-step meetings—are a powerful way to manage stress and maintain emotional balance. The sense of fellowship, support, and camaraderie at meetings can lend stability to your life, even when everything else feels uncertain.
Even studies show that “people power” - the kind you discover when you’re at a 12-step meeting or recovery-related event - actually contributes to better outcomes for people in sobriety. Long-term research has shown that people who attend 12-step meetings regularly - up to three times a week or more - stay sober for much longer than those who don’t, often up to 16 years or more without a relapse.
(more…)
Life in recovery can feel overwhelmingly difficult at times. We live in a stressful era and often don’t notice stress building up until it’s too late. The temptation to isolate can be hard to resist, and this allows many people to pursue their addiction in private. Support groups can be a key part of any successful relapse prevention effort.
Humans are social creatures, and addiction often takes away some of that humanity. It can fill the addicted person with shame and self-loathing. It can isolate people from their loved ones and keep them from doing things they enjoy.
In recovery, activities with other recovering people can be the glue that holds your new life together. Support groups—especially 12-step meetings—are a powerful way to manage stress and maintain emotional balance. The sense of fellowship, support, and camaraderie at meetings can lend stability to your life, even when everything else feels uncertain.
Even studies show that “people power” - the kind you discover when you’re at a 12-step meeting or recovery-related event - actually contributes to better outcomes for people in sobriety. Long-term research has shown that people who attend 12-step meetings regularly - up to three times a week or more - stay sober for much longer than those who don’t, often up to 16 years or more without a relapse.
(more…)When You Get in a Car Wreck: The Role of Specialized Chiropractic Care
Recognizing the Signs of Alcoholism: A Guide to Understanding Symptoms
- Drinking alcohol in larger amounts or over a longer period than intended.
- Craving alcohol.
- Developing a tolerance, requiring more alcohol to achieve the same effects.
- Suffering from withdrawal symptoms when not drinking.
- Neglecting responsibilities at work, home, or school due to drinking behavior.
- Engaging in risky behaviors while under the influence, such as driving or unsafe sexual activity.
Understanding Alcohol Use Disorder
Alcohol use disorder is a medical condition formally recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). It encompasses a spectrum of problematic drinking habits, ranging from mild to severe. People with AUD often struggle with an impaired ability to control their alcohol consumption, even when facing health problems or damage to relationships. Heavy drinking and frequent binge episodes, defined as consuming five or more drinks for men or four or more for women in about two hours, poses a significantly increased risk of developing AUD. Family history of substance abuse or mental disorders also raises susceptibility. (more…)How to Balance Work, Life, and Recovery in a Palm Springs Sober Living Home
Whether you’re attending meetings, exploring the desert landscape, or simply enjoying the peace of your sober living home, every small...
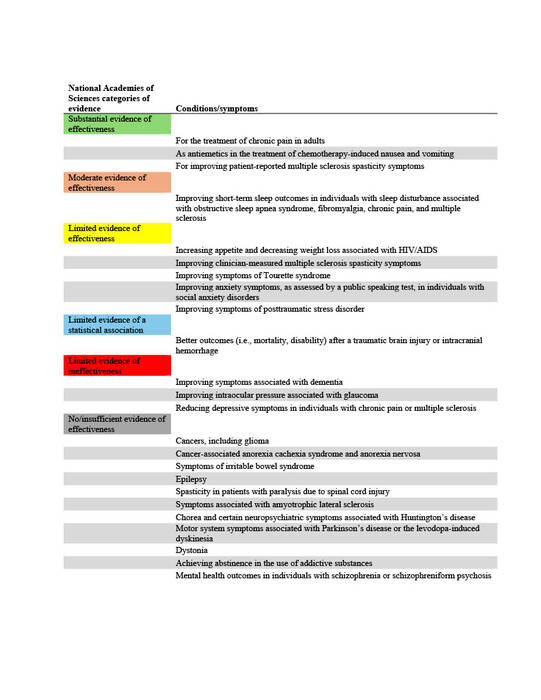
Evidence-Based Medicine Up in Smoke? An Analysis of the Qualifying Conditions for Medical Marijuana
The Role of Genetics in Substance Use Vulnerability and Recovery
Genetic Factors in Addiction Risk
Research indicates a significant link between genetics and the risk of developing substance use disorders. Genes play an impactful role, contributing to approximately 40-60% of the predisposition to addiction. Certain gene variations, such as those found in dopamine receptor genes, can enhance this likelihood. The presence of similar disorders in a family history can point to a potential genetic predisposition. This genetic influence is prominently observed in substance dependencies like alcohol and nicotine. Nevertheless, the role of environmental factors in interacting with these genetic risks mustn't be neglected. Gaining an understanding of the interplay between genetics and addiction contributes to our knowledge of this multifaceted matter. (more…)Top Evidence-Based Treatment for Addiction: Strategies That Work
No two individuals experience addiction in the same way. Effective substance abuse treatment must be personalized, taking into account factors...
Overcoming Stigma: Why Seeking Drug Rehab is a Sign of Strength
Breaking the Silence: Sharing Success Stories to Inspire Change
One of the most potent ways to combat the stigma of drug rehab is through the sharing of success stories. These narratives of triumph offer hope, shatter misconceptions and illuminate the realities of addiction and recovery. Each story underscores the transformative power of rehabilitation and the resilience inherent in the human spirit. Success stories serve as a beacon for those who are still hesitant to seek help. By highlighting the journey of those who have walked the path of recovery, individuals can find the encouragement and motivation to empower themselves. It is an acknowledgment that while addiction is a part of their story, it does not define their entire identity or their future. A New Found Life reclaimed through the process of drug rehab, carries with it invaluable lessons and experiences. In sharing these journeys, those in recovery can challenge prevailing biases and illustrate that rehabilitation and a return to a fulfilling life are within reach. Celebrating these victories amplifies the message that recovery is possible and worthy of pursuit. (more…)The Importance of Medically Supervised Drug Detox Treatment
Long-term recovery outcomes improve when detox is conducted under medical supervision. Proper stabilization enhances the transition into rehabilitation programs, increasing...
Teen Rehab: How Social Media Addiction and Substance Abuse Are Linked
The Unspoken Link Between Social Media and Addiction
Teenagers are very sensitive; hence, social media is a main influence weapon. Studies reveal that overuse of screens could cause mental problems like poor self-esteem, anxiety, and sadness. However, the connection between drug use and social media addiction goes well beyond what most individuals would consider. These two are connected, thus:- Contact with Substance Abuse
- Online challenges and peer pressure
- Mental Health Decline Producing Self-Medication
- Dopamine Demand and Enhanced Addiction Risk
Natural Pain Relief Without Risks from Opioids
Many countries have been grappling with an opioid crisis, which has motivated patients to seek cannabis as a much safer alternative. Medicinal cannabis minimizes the risks of addiction associated with opioids due to misuse and gives little risk of an overdose. To obtain medicinal cannabis legally, there are options like medical marijuana cards you can obtain from providers such as Leafy Doc Mississippi. Regarding how cannabis works in terms of pain relief, cannabinoids like THC bind to receptors in the brain and the immune system, modulating the experience of pain. The endocannabinoid system engages with trauma states mainly on account of pain, mood regulation, and inflammation. However, for long-term relief, medicinal cannabis is viewed as a considerably safer alternative compared to opioids. (more…)Addiction Recovery and Brain Health: The Role of Sober Living in Neurological Healing
The Brain’s Recovery Process After Addiction
Substance use alters the brain’s reward system by overstimulating dopamine production, leading to cravings and dependency. Prolonged use also damages the prefrontal cortex, which governs rational thinking and impulse control. Even after stopping substance use, the brain needs time to repair these functions, and the right environment is key to facilitating this process. Early recovery is often marked by post-acute withdrawal syndrome (PAWS), which can include mood swings, anxiety, and cognitive fog. Research shows that a stable living environment can help reduce these symptoms by providing consistency and reducing exposure to triggers. Without external stressors like unsafe housing or exposure to substance use, the brain can focus on healing neural pathways and restoring equilibrium. (more…)Hills Recovery: The Healing Power of Being Heard
 For many who turn to alcohol or drugs, the deeper problem lies in feeling ignored or misunderstood.
In this heartfelt video segment, Vanessa highlights, “Most people who turn to alcohol and drugs to cope… they’ve never really had a sounding board.” This statement captures the profound loneliness that can exacerbate addictive behaviors.
When individuals finally encounter a place where sharing is encouraged and valued, the impact can be transformative. The weight of shame and isolation begins to lift when someone feels truly listened to. This newfound sense of validation can, in turn, become the catalyst for more profound emotional healing.
(more…)
For many who turn to alcohol or drugs, the deeper problem lies in feeling ignored or misunderstood.
In this heartfelt video segment, Vanessa highlights, “Most people who turn to alcohol and drugs to cope… they’ve never really had a sounding board.” This statement captures the profound loneliness that can exacerbate addictive behaviors.
When individuals finally encounter a place where sharing is encouraged and valued, the impact can be transformative. The weight of shame and isolation begins to lift when someone feels truly listened to. This newfound sense of validation can, in turn, become the catalyst for more profound emotional healing.
(more…)Understanding Insurance and Addiction Treatment
Drafting a well-informed appeal letter is often the first step in challenging a denial. Your appeal should include evidence of...