This post discusses mental health.
- If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat at org. To learn how to get support for mental health, drug or alcohol conditions, visit FindSupport.gov. If you are ready to locate a treatment facility or provider, you can go directly to FindTreatment.govor call 800-662-HELP (4357).
- S. veterans or service members who are in crisis can call 988 and then press “1” for the Veterans Crisis Line. Or text 838255. Or chat online.
- The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
Why are more people experiencing anxiety? Stressful lifestyles and uncertain times often contribute to rising mental health challenges. Fortunately, effective treatments are available to provide relief and support. Let us explore why anxiety is a growing concern and how treatment can help.
Understanding the Rise in Anxiety
Many individuals struggle with anxiety due to various factors. Increased anxiety from work, family responsibilities, and economic pressures often play a role.
Anxiety treatment Lakewood professionals has observed that societal changes also contribute to heightened mental health issues.
Social isolation, digital pressures, and health concerns increase emotional challenges. With proper care, professionals can address these root causes, offering effective support. Awareness of these issues is the first step toward improvement.
Common Symptoms of Anxiety
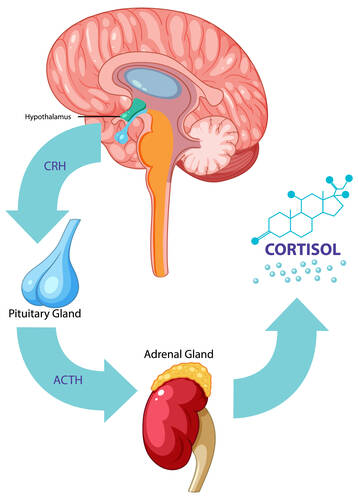
Symptoms can range from mild to severe, affecting daily life, and recognizing them is essential for seeking help in significant ways. Physical symptoms like fatigue, restlessness, and muscle tension are common. Emotional signs include excessive worry, irritability, and feelings of dread.
Anxiety can cause concentration issues, disrupted sleep, and behavioral changes, such as avoiding certain situations. These symptoms impact relationships, work, and overall well-being. Recognizing these signs encourages individuals to seek help, and early intervention leads to better outcomes. Understanding treatment options is crucial for managing and alleviating anxiety effectively.
(more…)