Gastrointestinal Disease, Microbiome, Probiotics, Supplements, Weight Research / 03.12.2024
Gut Health and Appetite Regulation: How Your Microbiome Influences Hunger
Editor's note: Please consult with your health care provider before using any supplements including probiotics.
Side effects are uncommon but may occur.
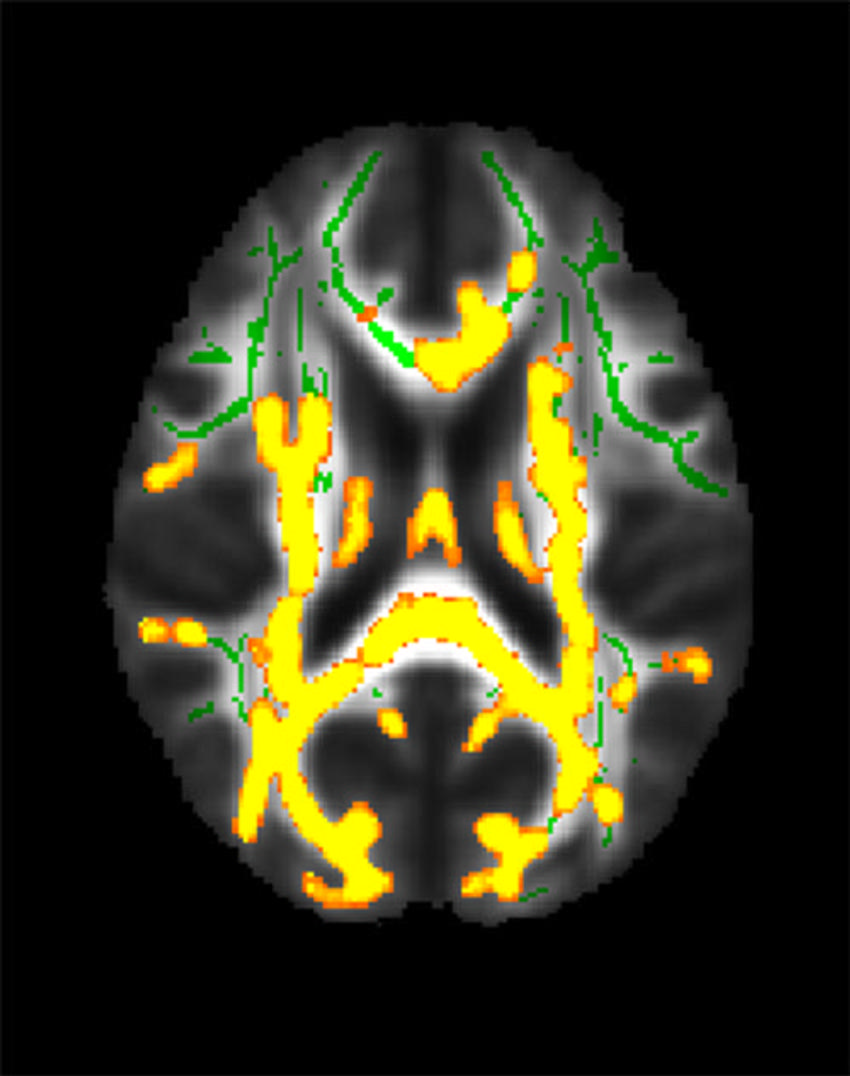
The connection between the gut and the brain is one of the most fascinating areas of research in recent years, with scientists uncovering how the microbiome—the trillions of microorganisms residing in our digestive system—can affect not just our digestion and immune system but also our feelings of hunger and satiety. As the science behind the gut-brain axis continues to unfold, it’s becoming increasingly clear that the health of our gut microbiome plays a pivotal role in regulating appetite, food intake, and body weight.
Understanding the intricate relationship between gut health and appetite regulation has profound implications for combating obesity, overeating, and eating-related disorders. In this article, we’ll explore how the microbiome influences hunger, the role it plays in appetite regulation, and what you can do to optimize gut health for better control over your hunger and eating habits. We will also look at products which aim to support a healthy microbiome and improve overall well-being.