Alzheimer's - Dementia, Author Interviews, Weight Research / 28.11.2023
RSNA23: WashU Study Finds Link Between Hidden Belly Fat and Alzheimer’s Disease
MedicalResearch.com Interview with:
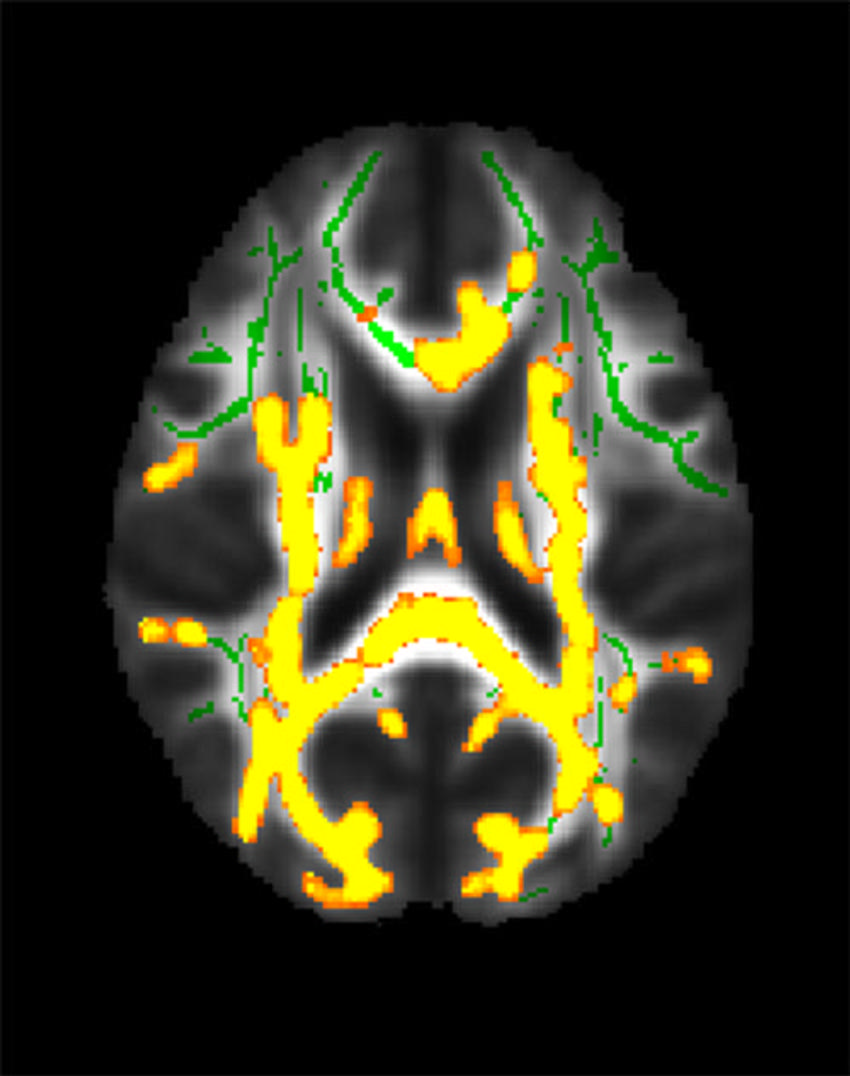
Mahsa Dolatshahi, M.D., M.P.H. Post-doctoral research fellow Mallinckrodt Institute of Radiology (MIR) Washington University School of Medicine St. Louis MedicalResearch.com: What is the background for this study? Response: Obesity at midlife is recognized as a risk factor for developing Alzheimer disease decades afterwards. However, body mass index on its own does not adequately represent the risks associated with obesity. In this study, we went beyond BMI and considered anatomical distribution of body fat, including the metabolically active visceral fat in the belly, and showed its association with Alzheimer pathology in the form of amyloid proteins. In addition, visceral fat along with obesity and insulin resistance were associated with thinning of brain cortex, as early as midlife. (more…)