A New Era in Pain Relief How Stem Cell Therapy Alleviates Back Pain


One of the best things you can do for sciatica is to keep moving, even if it’s the last thing...
Minimally invasive spine surgery (MISS) has become a game changer in orthopedic surgery, offering patients safer and less painful options for treating spinal issues. Dr. Brent Felix, a leading orthopedic spine surgeon, is at the forefront of this movement, advocating for these innovative techniques that provide multiple benefits over traditional methods.
Minimally invasive spine surgery, or MISS, is a technique that allows surgeons to address spine conditions with much smaller incisions compared to traditional surgery. Rather than making large cuts to access the spine, Dr. Felix and his team use special instruments and imaging tools to perform surgery through small incisions. These tools include tiny cameras or endoscopes, which provide a clear view of the spine without the need for large openings.
(more…)Spinal stenosis affects millions of people and its symptoms can range in severity, with some people not even knowing they...
 Most news stories tend to focus on how drugs and the opioid epidemic are impacting people in their teens and early adulthood. However, I can tell you from personal experience, that there are a lot of older adults who are also abusing drugs alcohol at record rates. This is borne out at our family’s drug treatment program which I founded and run in San Diego, California.
You may be surprised to hear that the rates of opioid overdose in the U.S. have increased the most among people ages 65 and up (from 2021 to 2022) and that older adults have seen the greatest increase in cannabis use in Canada. One thing you also may not realize is that older adults have the highest recovery rates of all age groups.
(more…)
Most news stories tend to focus on how drugs and the opioid epidemic are impacting people in their teens and early adulthood. However, I can tell you from personal experience, that there are a lot of older adults who are also abusing drugs alcohol at record rates. This is borne out at our family’s drug treatment program which I founded and run in San Diego, California.
You may be surprised to hear that the rates of opioid overdose in the U.S. have increased the most among people ages 65 and up (from 2021 to 2022) and that older adults have seen the greatest increase in cannabis use in Canada. One thing you also may not realize is that older adults have the highest recovery rates of all age groups.
(more…)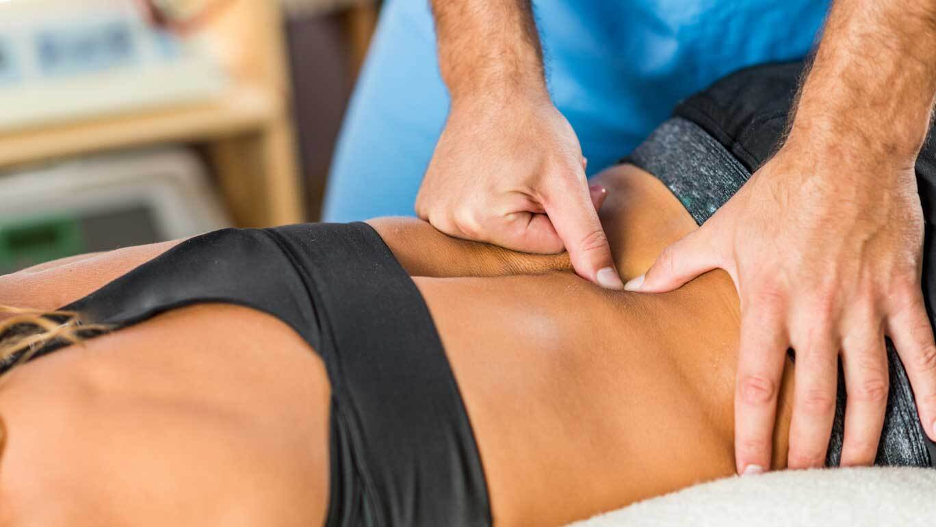 Pain management is a crucial aspect of maintaining a healthy and active lifestyle. While there are various methods to alleviate pain, topical gels have gained popularity due to their targeted approach and ease of use. Here are some of the key benefits of using topical gels for pain relief:
Pain management is a crucial aspect of maintaining a healthy and active lifestyle. While there are various methods to alleviate pain, topical gels have gained popularity due to their targeted approach and ease of use. Here are some of the key benefits of using topical gels for pain relief:
Don't hesitate to schedule a consultation with a qualified healthcare professional like an orthopedist specializing in spine care to discuss...
 The unpleasant sensation of chronic pain can have a considerable impact on an individual's life. Frequently lasting for months or years, chronic can affect individuals in any part of the body and for a variety of reasons. Chronic pain conditions affect a large number of Americans, who are left with no choice but to resort to various alternative medicines and physiotherapy.
This blog reflects the professional opinions of several pain management doctors and discusses their professional opinions regarding pain management techniques and treatments. Effective pain management hinges on a comprehensive approach that involves medication and appropriate therapy.
Let us explore some of the best practices for pain management.
The unpleasant sensation of chronic pain can have a considerable impact on an individual's life. Frequently lasting for months or years, chronic can affect individuals in any part of the body and for a variety of reasons. Chronic pain conditions affect a large number of Americans, who are left with no choice but to resort to various alternative medicines and physiotherapy.
This blog reflects the professional opinions of several pain management doctors and discusses their professional opinions regarding pain management techniques and treatments. Effective pain management hinges on a comprehensive approach that involves medication and appropriate therapy.
Let us explore some of the best practices for pain management.
 Although chiropractic care originated in China and Greece thousands of years ago, the practice of chiropractic care was formalized in 1895 in Iowa by D.D. Palmer when he manipulated a spine for a patient who was then healed of deafness and pain. Today, the advances in chiropractic training and experience have resulted in vastly-improved health outcomes and pain-free living for individuals worldwide.
Most people know how to find a good physician, but what elements are important in chiropractic care? What helps determine whether you will receive the care you need or not? If you ask friends for chiropractor recommendations, you may hear that one friendly chiropractor has a convenient office in the neighborhood, while another will recommend a female chiropractor who offers holistic care far beyond the basics. What elements should be included in effective chiropractic care?
Although chiropractic care originated in China and Greece thousands of years ago, the practice of chiropractic care was formalized in 1895 in Iowa by D.D. Palmer when he manipulated a spine for a patient who was then healed of deafness and pain. Today, the advances in chiropractic training and experience have resulted in vastly-improved health outcomes and pain-free living for individuals worldwide.
Most people know how to find a good physician, but what elements are important in chiropractic care? What helps determine whether you will receive the care you need or not? If you ask friends for chiropractor recommendations, you may hear that one friendly chiropractor has a convenient office in the neighborhood, while another will recommend a female chiropractor who offers holistic care far beyond the basics. What elements should be included in effective chiropractic care?
 Understanding the Latest Diagnostic Tools Enhancing Personal Injury Recovery
In the realm of personal injury recovery, precision in diagnosis is key. Advanced imaging techniques such as High-definition fiber tractography (HDFT) now allow for a superior visualization of neural pathways. Medical pros can pinpoint where you’re hurt with such precision, crafting a rehab plan that fits just right.
Thanks to biomarker technology, figuring out how long recovery will take has gotten a whole lot smarter. Imagine doctors using clues from your body’s own building blocks—genes and proteins—to create a recovery plan that’s all about you. It means less wondering, “Will this work?” and more knowing it will help stitch things back together quickly.
(more…)
Understanding the Latest Diagnostic Tools Enhancing Personal Injury Recovery
In the realm of personal injury recovery, precision in diagnosis is key. Advanced imaging techniques such as High-definition fiber tractography (HDFT) now allow for a superior visualization of neural pathways. Medical pros can pinpoint where you’re hurt with such precision, crafting a rehab plan that fits just right.
Thanks to biomarker technology, figuring out how long recovery will take has gotten a whole lot smarter. Imagine doctors using clues from your body’s own building blocks—genes and proteins—to create a recovery plan that’s all about you. It means less wondering, “Will this work?” and more knowing it will help stitch things back together quickly.
(more…) Chronic back pain troubles many people. Often, it seems as if there is hardly any relief available to them, but there is new research going on that promises better results - The BEST trial. Led by Dr Daniel Clauw from the University of Michigan, along with a team specializing in pain treatment, they aim to find effective strategies that can be custom-fit for distinct individuals suffering from back pain. Around 800 patients will participate in this process. BEST stands for Biomarkers for Evaluating Spine Treatments. It's part of the BACPAC Research Program and is supported by the National Institute of Arthritis and Musculoskeletal Skin Diseases through the NIH HEAL Initiative. The goal here is simple yet profound: Understand which treatment or combination works best depending on unique traits specific to patients. This bird’s eye perspective could benefit all chronic low back-pain sufferers across America. Their findings might link specific characteristics (known as biomarkers) with different treatments’ effectiveness levels thus helping doctors help patients better. If everything goes according to plan, every chronic lower-back pain patient may receive their tailored treatment, setting them up towards a recovery road.
Chronic back pain troubles many people. Often, it seems as if there is hardly any relief available to them, but there is new research going on that promises better results - The BEST trial. Led by Dr Daniel Clauw from the University of Michigan, along with a team specializing in pain treatment, they aim to find effective strategies that can be custom-fit for distinct individuals suffering from back pain. Around 800 patients will participate in this process. BEST stands for Biomarkers for Evaluating Spine Treatments. It's part of the BACPAC Research Program and is supported by the National Institute of Arthritis and Musculoskeletal Skin Diseases through the NIH HEAL Initiative. The goal here is simple yet profound: Understand which treatment or combination works best depending on unique traits specific to patients. This bird’s eye perspective could benefit all chronic low back-pain sufferers across America. Their findings might link specific characteristics (known as biomarkers) with different treatments’ effectiveness levels thus helping doctors help patients better. If everything goes according to plan, every chronic lower-back pain patient may receive their tailored treatment, setting them up towards a recovery road.A chiropractor can teach exercises to loosen up muscles and joints as well as perform the relevant procedures to reduce...
So many people are interested in finding alternatives to pain relief. Chiropractic treatment is just one of the many treatment...
