Anemia, Author Interviews, JAMA, OBGYNE / 23.08.2024
USPSTF Evaluates Screening and Supplementation for Iron Deficiency and Iron Deficiency Anemia During Pregnancy
Esa M. Davis, M.D., M.P.H , F.A.A.F.P
Professor of Medicine and Family and Community Medicine
Associate Vice President of Community Health and
Senior Associate Dean of pPopulation Health and Community Medicine
University of Maryland School of Medicine
Dr. Davis joined the U.S. Preventive Services Task Force in January 2021
MedicalResearch.com: What is the background for this study? What are the main findings?
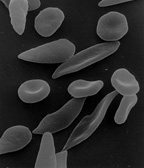
Response: Iron is important to overall health, and people need more iron when they are pregnant. This can make pregnant people at increased risk for iron deficiency, which can progress to anemia and cause complications for both moms and their babies. After reviewing the latest available research, the Task Force found that there is not enough evidence on whether pregnant people who do not have signs or symptoms of iron deficiency or anemia should be screened—or take iron supplements—to improve their health or the health of their baby. (more…)



 Bone marrow aspiration is a medical procedure where a small amount of the liquid part of your bone marrow is removed for examination. A
Bone marrow aspiration is a medical procedure where a small amount of the liquid part of your bone marrow is removed for examination. A 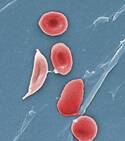


 Prof. Hiddo Lambers Heerspink, PhD PHARMD
Department of Clinical Pharmacy and Pharmacology
University Medical Center Groningen
Groningen
Prof. Hiddo Lambers Heerspink, PhD PHARMD
Department of Clinical Pharmacy and Pharmacology
University Medical Center Groningen
Groningen