Why Medical Bills Are Often a Surprise
Medical billing in the U.S. can be complex and opaque. Even with insurance, out-of-pocket costs can catch patients off guard. Common reasons for surprise bills include:- Out-of-Network Providers: Even during planned procedures, patients may unknowingly receive care from out-of-network specialists, resulting in much higher costs.
- High Deductibles: Many insurance plans come with deductibles that must be met before coverage kicks in, leaving patients to cover significant costs upfront.
- Ambulance Services: Emergency transportation is often not fully covered, leading to bills that average hundreds or even thousands of dollars.
- Hidden Fees: Charges for tests, medications, or consultations may not be clearly communicated beforehand.
Canadian Medications Offer Affordable Diabetic Options
Security and data protection are priorities in any online transaction, especially for healthcare. This pharmacy’s website is equipped with advanced...
Insulin Supplier: Accessible Diabetes Care for Everyone
Access to affordable insulin remains a challenge for millions of people living with diabetes around the world, particularly in middle-income countries. To bridge this gap, platforms are emerging that connect patients with high-quality insulin at reduced prices. For individuals struggling to afford their life-saving medication, these services offer a convenient and affordable solution, making a significant impact on global health.
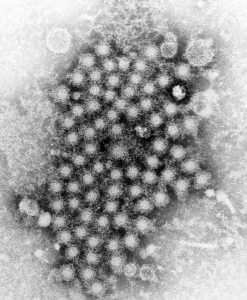
The Global Insulin Crisis
Diabetes affects millions worldwide, and the demand for insulin continues to rise. Major insulin manufacturers, including Novo Nordisk, Eli Lilly, and Sanofi, dominate the global market, producing essential medications for managing blood sugar levels. However, in many parts of the world, including countries like India, Mexico, and the Philippines, insulin prices remain prohibitively high. This leaves a substantial portion of the population without access to the medication they need to live healthy lives. Data shows that insulin prices are often out of reach for people in middle-income countries. The situation is particularly dire in regions like Kenya, Malaysia, and Vietnam, where the cost of insulin may equal a month's salary. With nearly three major companies controlling the insulin market, competition is limited, and prices remain high. As a result, many patients with type 1 and type 2 diabetes face inconsistent access to insulin, which can put their health at significant risk. (more…)Wasted Alzheimer’s Drug Can Cost Medicare Hundreds of Millions Annually
 As healthcare continues to evolve, more attention is being given to senior health, and wellness programs are increasingly becoming a cornerstone of comprehensive senior care.
Wellness programs focus on improving quality of life and managing chronic conditions through proactive measures such as exercise, nutrition, mental health support, and preventive care.
For seniors, these programs are especially valuable because they address the unique challenges that come with aging. As part of senior health plans, wellness programs are not only a way to treat existing issues but also a way to prevent future problems by promoting healthy lifestyles.
These programs offer a broad range of benefits, from improved physical health to enhanced mental well-being. Seniors enrolled in wellness initiatives often experience better control of conditions such as diabetes, heart disease, and arthritis.
In addition, wellness programs can help reduce hospital visits, lower healthcare costs, and increase overall longevity by encouraging proactive health management. Seniors who engage in regular fitness activities, for instance, are less likely to experience falls, fractures, and other mobility-related issues, which are common concerns in older age.
(more…)
As healthcare continues to evolve, more attention is being given to senior health, and wellness programs are increasingly becoming a cornerstone of comprehensive senior care.
Wellness programs focus on improving quality of life and managing chronic conditions through proactive measures such as exercise, nutrition, mental health support, and preventive care.
For seniors, these programs are especially valuable because they address the unique challenges that come with aging. As part of senior health plans, wellness programs are not only a way to treat existing issues but also a way to prevent future problems by promoting healthy lifestyles.
These programs offer a broad range of benefits, from improved physical health to enhanced mental well-being. Seniors enrolled in wellness initiatives often experience better control of conditions such as diabetes, heart disease, and arthritis.
In addition, wellness programs can help reduce hospital visits, lower healthcare costs, and increase overall longevity by encouraging proactive health management. Seniors who engage in regular fitness activities, for instance, are less likely to experience falls, fractures, and other mobility-related issues, which are common concerns in older age.
(more…)Generic vs Brand-Name Medication: What’s the Difference
 When you’re at the pharmacy, it’s normal to feel a bit of confusion about whether you would like to receive generic or brand-name medication when the pharmacy technician asks you the usual question. While health professionals, from pharmacists to doctors, nurses, and students of RN to MSN programs, will understand the differences between the two, it's important that you, as a patient, know them, too.
In this article, we will break down the differences between generic and brand-name medications so that you will be more aware when you visit the pharmacy.
When you’re at the pharmacy, it’s normal to feel a bit of confusion about whether you would like to receive generic or brand-name medication when the pharmacy technician asks you the usual question. While health professionals, from pharmacists to doctors, nurses, and students of RN to MSN programs, will understand the differences between the two, it's important that you, as a patient, know them, too.
In this article, we will break down the differences between generic and brand-name medications so that you will be more aware when you visit the pharmacy.
Why Retirees Must Enroll In Medicare During A Certain Time Frame What Is the Initial Enrollment Period (IEP)?
Texas A&M Studies Effect of Affordable Care Act on Uninsured Hospitalizations
Navigating Medicare: How to Find and Choose Primary Care Doctors
Understanding Medicare and Its Different Parts
Medicare is a federal health insurance program primarily for individuals aged 65 and older, though it also covers certain younger people with disabilities. Medicare consists of four parts:- Medicare Part A: Covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
- Medicare Part B: Covers certain doctors' services, outpatient care, medical supplies, and preventive services.
- Medicare Part C (Medicare Advantage): An alternative to Original Medicare that offers all Part A and Part B services through private insurance companies. These plans often include additional benefits like vision, dental, and prescription drug coverage.
- Medicare Part D: Covers prescription drugs.
Healthcare Payer: A Definition and What You Need to Know
Individual healthcare experience is greatly dependent on the healthcare payer they choose or rely on. Things like access to certain...
Virtual Patient Coordinators: A Game-Changer for Busy Medical Practices
Automated Eligibility Coverage Tracking Platforms: A Game Changer for Billing and Revenue Recovery?
The Problem: Manual Tracking Just Doesn't Cut It Anymore
Determining a patient’s status as well as his or her insurance is a crucial but time-consuming process in the billing department. Previously, it included calling insurance companies, verifying the data in different systems, and entering the information into spreadsheets. Since patient details are dynamic and various claims need to be addressed every week, it becomes impossible to manage information updates through traditional methods. Some of the problems include:- Time-Consuming Process - Verifying coverage manually can take up to 30 minutes per patient. For large billing companies, this may translate into big time losses.
- Human Error - Manually compiling and updating records inevitably leads to inaccurate or outdated information falling through the cracks.
- Claim Denials - Incorrect policy details lead to higher denial rates, payment delays and lost revenue.
- Lack of Visibility - With records scattered across systems and spreadsheets, billing teams lack clear visibility into coverage changes.
Brown University Study Finds No Increase in Home Dialysis or Kidney Transplantation with Government’s Pay-For-Performance Program
DDW24: Study Suggests Female GI Physicians Are Better Meeting the Care Needs of their Patients
Dialysis Facilities Serving Disadvantaged Populations More Frequently Penalized Under Pay-For-Performance Model
Pharmacy Forecast: Paradigm Shifts in Breakthrough Therapeutics Will Challenge Existing Payment Models
Study Finds Re-dispensing Unused Cancer Drugs Can Save Money and the Environment
 Lisa-Marie Smale, PharmD
Lisa-Marie Smale, PharmDPhD Candidate Clinical Pharmacy
Radboud University Medical Center
Department of Pharmacy
Nijmegen, the Netherlands MedicalResearch.com: What is the background for this study? Response: Cancer drugs are not always fully used by patients, while these drugs are mostly expensive and environmentally damaging, both in production and (waste) disposal. Therefore we investigated whether unused drugs of patients can be collected, verified of quality by a pharmacy, to be redispensed to other patients instead of being disposed of. We were interested whether such an approach ultimately leads to lower environmental impacts and costs. (more…)
New Alzheimer Drug Lecanemab and its Ancillary Services Could Cost Medicare up to 5 billion Annually
 John N. Mafi, MD, MPH
Associate Professor of Medicine
General Internal Medicine & Health Services Research
David Geffen School of Medicine at UCLA
MedicalResearch.com: What is the background for this study? What is lecanemab used for and how well does it work?
Response: Lecanemab is a treatment for mild cognitive impairment and mild dementia that was approved in January 2023 as part of the Food and Drug Administration’s (FDA) accelerated approval program. The results from a recent phase 3 clinical trial show a modest clinical benefit: the rate of cognitive decline by 27% in an 18-month study involving participants experiencing the early stage of Alzheimer’s, with an 0.45-point absolute difference in cognitive testing scores. However, due to the risk of brain swelling and bleeding (also known as amyloid-related imaging abnormalities), treatment with lecanemab involves frequent MRIs and neurology or geriatrics appointments to monitor for these abnormalities, which can be life threatening. So far, three patient deaths have potentially been tied to lecanemab.
It is likely that the FDA will grant is lecanemab traditional approval later this year, prompting Medicare to reconsider its current coverage restrictions and potentially enabling widespread use.
(more…)
John N. Mafi, MD, MPH
Associate Professor of Medicine
General Internal Medicine & Health Services Research
David Geffen School of Medicine at UCLA
MedicalResearch.com: What is the background for this study? What is lecanemab used for and how well does it work?
Response: Lecanemab is a treatment for mild cognitive impairment and mild dementia that was approved in January 2023 as part of the Food and Drug Administration’s (FDA) accelerated approval program. The results from a recent phase 3 clinical trial show a modest clinical benefit: the rate of cognitive decline by 27% in an 18-month study involving participants experiencing the early stage of Alzheimer’s, with an 0.45-point absolute difference in cognitive testing scores. However, due to the risk of brain swelling and bleeding (also known as amyloid-related imaging abnormalities), treatment with lecanemab involves frequent MRIs and neurology or geriatrics appointments to monitor for these abnormalities, which can be life threatening. So far, three patient deaths have potentially been tied to lecanemab.
It is likely that the FDA will grant is lecanemab traditional approval later this year, prompting Medicare to reconsider its current coverage restrictions and potentially enabling widespread use.
(more…)Inflation Reduction Act: Implications on Out-Of-Pocket Costs for Patients with Heart Disease Risk Factors
Yale Study Finds Pharmaceutical Companies Focus Advertising On Expensive Brand-Name Drugs
Physician Weekly Work Hours Fall Especially for Doctor Fathers
SLE – Lupus: Size of Copay Influences Medication Adherence
Hepatitis C: Few Insured Persons Receive Timely Treatment, and Disparities Exist
Covid: Safety Net Hospitals Experienced Greater Financial Losses During Pandemic
Allison Witman PhD Assistant Professor of Economics Economics & Finance Cameron School of Business University of North Carolina, Wilmington
Yu Wang PhD Assistant Professor Congdon School of Supply Chain, Business Analytics, & Information Systems Cameron School of Business University of North Carolina Wilmington David Cho PhD Assistant Professor of Management California State University, Fullerton
MedicalResearch.com: What is the background for this study? Response: The COVID-19 pandemic placed tremendous financial pressure on hospitals. Beginning in March of 2020, hospitals cancelled outpatient and elective procedures to accommodate surges in demand from COVID-19 patients. As these procedures account for more than 60% of an average hospital’s revenue, cancellation posed serious challenges to the financial health of hospitals. Revenue from COVID-19 patients may have partially offset these effects, but the American Hospital Association estimated a total loss of $202.6 billion by American hospitals between March and June 2020. In response, the U.S. government created large federal assistance programs aimed to stabilize hospitals’ financial situation as their ability to maintain operations was critical to the health of the nation. Due to differences in hospital characteristics, certain hospitals such as rural hospitals and those serving a higher share of Medicaid and uninsured patients (e.g., safety net hospitals) may have been more financially susceptible to the effects of the pandemic. These hospitals that serve vulnerable patient populations historically have had lower profit margins and were candidates for targeted COVID relief funding (e.g., Safety Net Hospitals Payments, a $10 billion component of the Provider Relief Fund). (more…)