The opioid crisis has left an indelible mark on society, affecting millions of individuals and families across the globe. While the physical and psychological tolls of opioid addiction are well-documented, another profound challenge often lurks in the shadows: the stigma surrounding opioid use disorder (OUD). Stigma, which manifests as judgment, discrimination, and negative perceptions, can be one of the most significant barriers to seeking treatment and achieving recovery. Overcoming this stigma is crucial for creating a supportive environment that encourages individuals to pursue and sustain their recovery journey.
Understanding Stigma in Opioid Addiction
Stigma can be defined as a set of negative beliefs or attitudes directed toward a particular group of people. In the context of opioid addiction, it often revolves around misconceptions that individuals suffering from OUD are morally flawed, weak-willed, or choosing to engage in substance use. These harmful stereotypes perpetuate a culture of shame and silence, discouraging people from seeking help for fear of being judged or ostracized.
The stigma around opioid addiction is fueled by various factors. Historically, addiction was viewed as a moral failing or criminal behavior rather than a medical condition. This perception persists, even though extensive research has shown that opioid addiction is a chronic brain disease influenced by genetics, environment, and mental health. Additionally, sensationalized media coverage of drug-related crimes and overdose deaths further reinforces negative stereotypes, casting individuals with OUD in a criminalized light.
(more…)


 Elena Stains
Medical Student
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA
MedicalResearch.com: What is the background for this study?
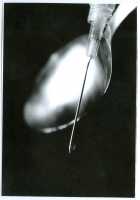
Response: Opioid use has been an increasing problem since the early 2000s in the United States (US) with a surge around 2010. Twenty-five percent of those having abused pain relievers in 2013 and 2014 got those drugs from physicians1. Physicians are particularly well-known for fueling the opioid crisis in Florida in the 2000s. Of the United States’ top 100 opioid prescribing physicians in 2010, an astounding 98 were prescribing in Florida2. Florida taking the main stage of the opioid crisis can be attributed to several factors, including ability of physicians to dispense opioids directly from their offices to patients (i.e. without pharmacists) and the presence of many infamous “pill mills” in the state3–6.
The researchers at Geisinger Commonwealth School of Medicine aimed to analyze the amount of hydrocodone (including brand names of Vicodin and Lortab) and oxycodone (OxyContin and Percocet) distributed in Florida from 2006 to 2021, paying close attention to the peak year of the opioid crisis, 2010. The team used the Washington Post and the US Drug Enforcement Administration’s Automation of Reports and Consolidated Orders System (ARCOS) databases to compile this compelling information.
Elena Stains
Medical Student
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA
MedicalResearch.com: What is the background for this study?
Response: Opioid use has been an increasing problem since the early 2000s in the United States (US) with a surge around 2010. Twenty-five percent of those having abused pain relievers in 2013 and 2014 got those drugs from physicians1. Physicians are particularly well-known for fueling the opioid crisis in Florida in the 2000s. Of the United States’ top 100 opioid prescribing physicians in 2010, an astounding 98 were prescribing in Florida2. Florida taking the main stage of the opioid crisis can be attributed to several factors, including ability of physicians to dispense opioids directly from their offices to patients (i.e. without pharmacists) and the presence of many infamous “pill mills” in the state3–6.
The researchers at Geisinger Commonwealth School of Medicine aimed to analyze the amount of hydrocodone (including brand names of Vicodin and Lortab) and oxycodone (OxyContin and Percocet) distributed in Florida from 2006 to 2021, paying close attention to the peak year of the opioid crisis, 2010. The team used the Washington Post and the US Drug Enforcement Administration’s Automation of Reports and Consolidated Orders System (ARCOS) databases to compile this compelling information.