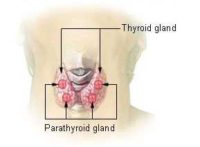
Author Interviews, Cancer Research, Endocrinology, JAMA, Pediatrics / 02.07.2018
Young Survivors of Cancer at Increased Risk of Endocrine Disease
MedicalResearch.com Interview with:
 Mette Vestergaard Jensen, MD
Danish Cancer Society Research Center
MedicalResearch.com: What is the background for this study?
Response: Cancer survival rates have improved and it is necessary to explore the long-term consequences of cancer treatment. Adolescents and young adults with cancer are at risk for several therapy-related late effects; however, these have not been studied extensively. We investigatet the lifetime risks of endocrine late effects of cancer and cancer treatment in adolescent and young adult cancer s
(more…)
Mette Vestergaard Jensen, MD
Danish Cancer Society Research Center
MedicalResearch.com: What is the background for this study?
Response: Cancer survival rates have improved and it is necessary to explore the long-term consequences of cancer treatment. Adolescents and young adults with cancer are at risk for several therapy-related late effects; however, these have not been studied extensively. We investigatet the lifetime risks of endocrine late effects of cancer and cancer treatment in adolescent and young adult cancer s
(more…)
 Mette Vestergaard Jensen, MD
Danish Cancer Society Research Center
MedicalResearch.com: What is the background for this study?
Response: Cancer survival rates have improved and it is necessary to explore the long-term consequences of cancer treatment. Adolescents and young adults with cancer are at risk for several therapy-related late effects; however, these have not been studied extensively. We investigatet the lifetime risks of endocrine late effects of cancer and cancer treatment in adolescent and young adult cancer s
(more…)
Mette Vestergaard Jensen, MD
Danish Cancer Society Research Center
MedicalResearch.com: What is the background for this study?
Response: Cancer survival rates have improved and it is necessary to explore the long-term consequences of cancer treatment. Adolescents and young adults with cancer are at risk for several therapy-related late effects; however, these have not been studied extensively. We investigatet the lifetime risks of endocrine late effects of cancer and cancer treatment in adolescent and young adult cancer s
(more…)