MedicalResearch.com Interview with:
Dr. Anna Plym PhD
Postdoctoral Research Fellow
Brigham and Women's Hospital
Harvard T.H. Chan School of Public Health
MedicalResearch.com: What is the background for this study? What are the main elements of the healthy lifestyle?
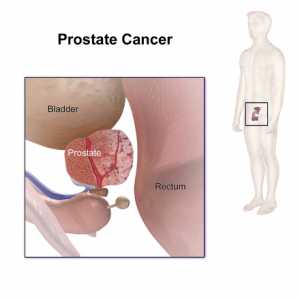
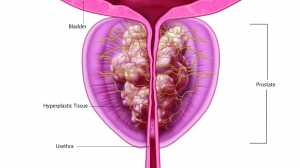
Response: Prostate cancer is the most heritable of all cancers, with genetic factors accounting for a large proportion of cases. Although we do not currently know about all the genetic factors contributing, a recent study identified 269 genetic markers for prostate cancer, validated in multiple independent populations (Conti et al., Nature Genetics 2021, Plym et al, JNCI, 2021:
https://academic.oup.com/jnci/advance-article-abstract/doi/10.1093/jnci/djab058/6207974). Based on a polygenic risk score derived from these 269 markers, we observed that men with a high polygenic risk score have over a 50% risk of developing prostate cancer within their lifetime. With this excess risk in mind, we were interested in possible ways in which the genetic risk of prostate could be attenuated. An increasing number of studies have suggested that lifestyle factors can affect the risk of lethal prostate cancer – however, these studies have seldom incorporated genetic factors. We know from other diseases that a healthy lifestyle is of benefit for individuals at high genetic risk, and we hypothesized that this would be the case for prostate cancer as well. In this study, we examined a healthy lifestyle score for lethal prostate cancer consisting of six components: healthy weight (BMI < 30), not smoking (never smoked or quit > 10 years ago), vigorous physical exercise (3 or more hours per week), high intake of tomatoes or tomato-based products (7 servings or more per week), high intake of fatty fish (1 or more serving per week) and low intake of processed meat (less than 3 servings/week of beef or pork hot dogs, bacon, salami, bologna, or other processed meat sandwiches) (Kenfield et al, JCO, 2016).
(more…)