Aging, Alzheimer's - Dementia, Author Interviews, Brigham & Women's - Harvard, Genetic Research, Nature / 20.04.2022
Neurons in Alzheimer’s Disease Have Different Mutations Than Those That Occur in Normal Aging
MedicalResearch.com Interview with:
Michael B. Miller, MD, PhD
Instructor, Harvard Medical School
Department of Pathology
Brigham and Women's Hospital
MedicalResearch.com: What is the background for this study? Would you explain what is meant by somatic genetic changes and how they might occur?
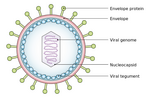
Response: Changes, also called mutations, in the DNA sequence of genes can be passed from parents to their children, and explain why many diseases run in families. This kind of DNA change is called a germline mutation and is present in every cell in a person’s body. Gene mutations can also occur in a subset of cells of a person, in which case they are called somatic mutations. Somatic mutations are well known as a cause of cancer, and recent research has found that somatic mutations can also happen in non-cancerous cells that appear otherwise normal. Recent studies have even found that somatic mutations are present in neurons, cells in the brain that transmit electrical signals and play an important role in how the brain functions. Furthermore, in neurons, somatic mutations increase with age, so we set out to understand if somatic mutations might be playing a role in age-related brain diseases like Alzheimer’s.
(more…)