Author Interviews, Mental Health Research, University of Michigan / 27.10.2024
Psychedelics: Adverse Events and Reports of Sexual Misconduct
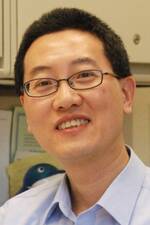
MedicalResearch.com Interview with:
Daniel J. Kruger, PhD
University of Michigan
MedicalResearch.com: What is the background for this study?
Response: A team of researchers from the University of Michigan and University at Buffalo teamed up with psychedelic advocates and therapists to document some of the challenges with psychedelics. They surveyed over a thousand psychedelic users about their adverse experiences and the experiences they have heard from others.
Most reported being frightened, sadness, loneliness, and feeling their body tremble or shake at times. Some people experienced panic, paranoia, felt that they are dead, or that the state they were in would last forever. One in ten participants had adverse physical reactions. For most people having these experiences, they are rare or happen sometimes, but they are still significant. Most of the people that experienced a severe adverse event did not have guidance from someone who was knowledgeable about psychedelics.
A small portion of participants knew about an incident of inappropriate sexual contact by a psychedelic sitter, guide, or practitioner, the perpetrators were mostly underground guides and friends or acquaintances.
(more…)



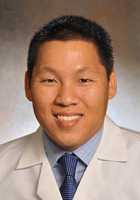
 Wilson N. Merrell
Ph.D. Student
Wilson N. Merrell
Ph.D. Student