MedicalResearch.com Interview with:
Dr. Fred Apple,
PhD, DABCC
Medical director,Clinical Laboratories, Clinical Chemistry, Clinical and Forensic Toxicology and Point of Care Testing, Hennepin HealthCare
Principal investigator, Minneapolis Medical Research Foundation
Professor, Department of Laboratory Medicine and Pathology
University of Minnesota
MedicalResearch.com: What is the background for this study?
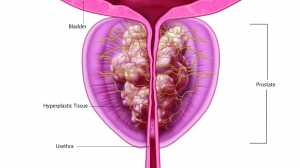
Response: Few studies have addressed the role of high sensitivity cardiac troponin (hs-cTn) assays in ruling out myocardial infarction (MI) based on the measurement of a single baseline specimen in US patients presenting to the emergency department with symptoms suggestive of ischemia. Most studies have been published predicated on patients in Europe, Australia, and New Zealand. As US emergency departments have different ordering practices for using cTn in triaging patients, it is important to validate the role of hs-cTn assays in US practices to assure providers of appropriate utilization. We have published two papers using the Abbott ARCHITECT hs-cTnI assay, the same one used outside the US in clinical practice (as this assay is not yet FDA cleared) in a US cohort (
clinicialtrials.gov trial: UTROPIA - Sandoval Y, Smith SW, Shah ASV, Anand A, Chapman AR, Love SA, Schulz K, Cao J, Mills NL, Apple FS.
Rapid rule-out of acute myocardial injury using a single high-sensitivity cardiac troponin I measurement. Clin Chem 2017;63:369-76. Sandoval
Y, Smith
SW, Love
SA, Sexter
A, Schulz
K, Apple
FS. Single high-sensitivity cardiac troponin I to rule out myocardial infarction. Am J Med 2017;130:1076-1083) that have shown similar rule out capacities predicated on clinical presentation, a normal ECG and the role of hs-cTnI testing.
(more…)
 Key Takeaways
Key Takeaways