Author Interviews, Breast Cancer, Colon Cancer, Genetic Research, JAMA / 20.06.2024
Lifetime Cancer Risk with Germline CDH1 Variants
MedicalResearch.com Interview with:
Dr. Jeremy L. Davis M.D.
Surgical Oncologist
Center for Cancer Research
Dr. Davis’ research focuses on sporadic and inherited forms of stomach cancer.
National Cancer Institute
MedicalResearch.com: What is the background for this study?
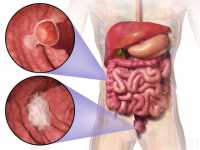
Response: Individuals who are born with a CDH1 gene mutation are at increased risk of developing specific cancers in their lifetime. Those cancers are called diffuse-type gastric cancer and lobular breast cancer.
The background that is relevant here is that when mutations in this gene were first identified as the cause of inherited forms of these cancers, the estimated lifetime risk of gastric cancer, for instance, was around 60-83%. Because of this very high risk and because gastric cancer is particularly difficult to treat, many experts recommend prophylactic surgery to remove the stomach. In recent years, as we have seen more families who carry a CDH1 gene mutation, we have also observed that gastric cancer rates did not seem quite as high as those risk estimates would have suggested. We sought to re-evaluate lifetime risk of cancer with a large and diverse cohort of individuals throughout North America.
(more…)