26 Dec Transforming Chronic Disease Management with a Touch of Technology
Chronic illness management has grown easier due to technological developments and inventive treatments. From wearable gadgets to real-time health tracking, technology is changing the way patients receive treatment. These advancements enable people to monitor and control their health proactively from home.
As healthcare providers adopt these tools, patient outcomes improve, and the burden on facilities decreases. With a focus on seamless communication, digital health tools foster stronger doctor-patient relationships.
In this article, we will explore how technology is revolutionizing chronic disease management, focusing on its practical applications and benefits. Let’s discuss five key ways technology is driving change.
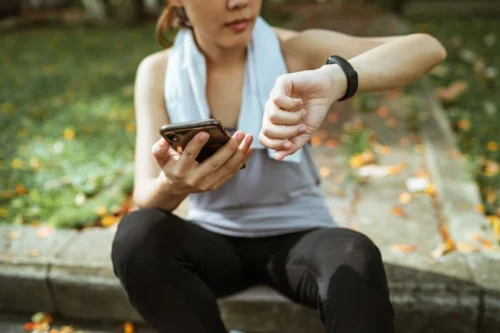
The Role of Wearable Technology
Wearable devices allow patients to track their health and exchange information with healthcare providers. These gadgets monitor vital indicators, physical activity, and even stress levels to provide real-time information.
HealthTech Magazine states that wearables improve health management by providing continuous tracking and personalized insights through companion applications.
Open APIs allow seamless data integration, linking devices like Apple Watch with Apple Health platforms. This infrastructure delivers actionable reminders to patients and provides providers with data for informed clinical decisions during appointments.
Wearables offer numerous benefits for both physicians and patients, including:
- Providing clinicians with useful information for accurate diagnosis and individualized treatment options.
- Encouraging patients to actively participate in their health management and enhance their overall wellness.
- Detecting early warning signs helps prevent complications from worsening over time.
Wearables are helping to bridge the gap between healthcare practitioners and people throughout the world.
What are the key benefits of using wearables in chronic care?
Wearables have significant advantages, such as continuous monitoring, early warning indications, and individualized therapy. They give crucial data that clinicians may use to make educated decisions. They also inspire patients to be proactive, which improves adherence to treatment programs and helps manage chronic illnesses more efficiently.
How Remote Patient Monitoring Redefines Chronic Care
According to CoachCare, remote patient monitoring (RPM) provides doctors with real-time health data without requiring hospital visits. Patients utilize linked gadgets to monitor vital indicators such as blood pressure and glucose levels. These readings are immediately communicated to healthcare practitioners for early action as needed.
Remote patient monitoring improves results by identifying possible health concerns before they become crises. It also allows patients to understand and control their ailments from the comfort of their own homes. RPM reduces healthcare expenses and enhances patient access by minimizing hospital visits.
TechTarget notes that remote patient monitoring (RPM) adoption has surged dramatically in recent years, experiencing a 1,294% increase. From January 2019 to November 2022, RPM claim volume skyrocketed, showcasing its growing popularity.
This rapid expansion reflects the growing need for new healthcare solutions that enhance patient care and expedite medical services.
Understanding How Remote Patient Monitoring Platforms Work
Remote patient monitoring platforms connect patients with healthcare providers through advanced digital health technologies. These platforms integrate connected devices like glucose monitors, blood pressure cuffs, and pulse oximeters. Data from these devices is transmitted securely to cloud-based systems for providers to analyze in real-time.
Physicians are alerted to abnormal data, allowing for quick treatments to avoid problems and hospitalizations. Patients use user-friendly mobile apps to track their metrics and receive personalized health insights daily. These platforms promote collaboration between patients and providers, enhancing overall care coordination and disease management.
Remote patient monitoring also enables continuous monitoring, ensuring that patients get care that is personalized to their changing health requirements. With the help of a remote patient monitoring platform, healthcare providers can review historical trends to adjust treatments based on long-term health patterns.
What is the benefit of real-time data analysis in remote monitoring?
Real-time data analysis allows healthcare providers to promptly address any abnormal readings, preventing complications. Immediate alerts to physicians enable quick interventions when necessary. This timely action improves patient outcomes by minimizing delays in care, especially for chronic conditions that require constant monitoring.
Analyzing Big Data for Better Patient Outcomes
Big data analytics is crucial for spotting patterns and anticipating health risks. Healthcare providers analyze large datasets to understand patient behaviors and treatment outcomes.
SpringerOpen mentions that healthcare data has grown exponentially with electronic medical records and patient-generated data from various sources.
Today, the industry generates large volumes of data, such as health records, medical photographs, and genetic information. Effective use of these data can improve clinical decision-making, disease monitoring, and public health management.
Predictive algorithms help identify individuals at risk of complications or disease progression. This allows for early interventions that improve long-term health outcomes for patients.
Data-driven insights also personalize treatments based on individual needs, improving effectiveness. Collaboration between healthcare institutions and tech companies ensures continuous improvement in data analysis capabilities.
How does big data personalize medical treatments?
Big data enables the personalization of treatments by analyzing individual patient health histories and behaviors. Physicians use this data to tailor treatments that best suit a patient’s needs. Big data improves the effectiveness and efficiency of medical care by offering more targeted interventions.
Mobile Apps as a Companion for Disease Management
Mobile health applications provide users with simple tools for recording drugs, visits, and health indicators. These applications provide patients with reminders to ensure they follow their treatment recommendations.
They also provide educational tools to assist patients in understanding their diseases. Many applications integrate with wearable devices, consolidating health data into a single platform.
As per Grand View Research, the global disease management apps market was valued at $9.94 billion in 2023. It’s projected to grow at a 12.1% CAGR from 2024 to 2030, driven by chronic disorders. Increased awareness of healthy lifestyles, alongside IT integration in healthcare, is fueling the adoption of mobile healthcare apps.
Real-time communication systems enable patients to consult with healthcare providers remotely when necessary. These apps’ user-friendly designs make them accessible to people of all ages and technical ability levels.
Can mobile apps improve disease awareness among patients?
Yes, many mobile health apps offer educational resources about specific diseases and treatment options. They help patients understand their conditions better, leading to informed decision-making. This increased awareness empowers patients to take a more active role in managing their health.
Improving Accessibility Through Telemedicine
Telemedicine allows people to consult with healthcare providers without the necessity for in-person appointments. Video consultations enable patients to discuss symptoms, treatment options, and future care plans.
Patients with chronic diseases can receive care even in distant places with minimal healthcare services. Telemedicine minimizes travel time, allowing patients to focus on their health without breaking their regular routines.
Telemedicine enables healthcare practitioners to monitor patient’s progress and adjust treatments as necessary. With continued technological advancements, telemedicine offers endless possibilities for enhancing patient care.
Can telemedicine improve healthcare access for non-English speakers?
Yes, telemedicine can improve access by offering language options and translation services during virtual consultations. This guarantees that patients who do not speak English can receive care without encountering linguistic obstacles. Telemedicine makes healthcare more inclusive, ensuring better access for diverse populations.
Technology is transforming chronic illness management by making it more proactive, tailored, and accessible. Empowering patients with self-monitoring devices enables them to manage their health at home. Remote care technology enables patients and providers to interact more effectively and achieve better outcomes. Data analytics helps adapt therapies, resulting in improved health outcomes.
This trend is altering healthcare, resulting in better patient-provider connections and adherence to treatment programs. With technology, chronic disease management is becoming more efficient and effective. The future promises a more equitable healthcare system where both patients and providers work together for optimal health outcomes.
—————————
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition.
Some links are sponsored. Products and services are not warranted or endorsed.
Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on December 26, 2024 by Marie Benz MD FAAD