
06 Aug Appreciable Continued Prescribing of Paroxetine, a Potentially Inappropriate Medicine, in People 65+

Luke Cavanah
Luke Cavanah, BS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 18509
MedicalResearch.com: What is the background for this study?
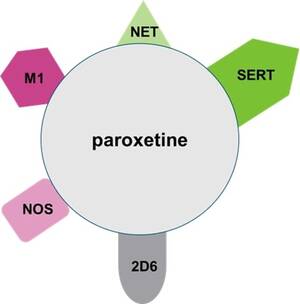
Response: “Selective” serotonin reuptake inhibitors (SSRI) are a class of medications that are first-line treatments for many anxiety, depressive, and other psychiatric disorders.1–3 Despite their name, SSRIs often have activity on other receptors and chemicals.4
One such SSRI that is known for being particularly nonselective is paroxetine.5 Paroxetine’s mechanisms of action are summarized in the figure below which shows binding not only to the serotonin transporter (SERT) but also to the norepinephrine transporter (NET), nitric oxide synthetase (NOS), the muscarinic (M1) receptor, and the liver cytochrome 2D6 enzyme. Paroxetine’s receptor promiscuity, especially its anticholinergic activity, can contribute to unfavorable adverse effects.5 Older adults (65+) are particularly vulnerable to some of these adverse effects.
The American Geriatrics Society (AGS) regularly publishes an explicit list, called the Beer’s List, of what they call “potentially inappropriate medications (PIMs)”, which are medications they recommend avoiding in this demographic when having certain disorders/conditions or most clinical contexts. The AGS Beers Criteria, in 2012, 2019, and most recently in 2023, has identified paroxetine as a PIM due to its strong anticholinergic activity and high risk of sedation and orthostatic hypotension, and thus they recommend it should be avoided in this population in most circumstances.6–8 Given the recommendation against the use of paroxetine in older adults, we were interested in examining the utilization of paroxetine by U.S. Medicare beneficiaries. Medicare patients primarily consist of people 65+ and cover 94% of non-institutionalized people in this age group.9
MedicalResearch.com: What are the key points of your research?
 Response: There were three key takeaways from the study of paroxetine use in the Medicare population from 2015 to 2020.
Response: There were three key takeaways from the study of paroxetine use in the Medicare population from 2015 to 2020.
First, despite the 2012 and 2019 AGS Beers’ Criteria recommending against the use of paroxetine in older adults in most circumstances, there was considerable, albeit declining (-34.52%), population-corrected use of paroxetine (2015: 122.61 prescr/thousand; 2020: 80.28 prescr/thousand).
Second, there was a consistent five-fold state-level variation in population-corrected paroxetine use for all years examined, which is unlikely to be fully explained by regional differences in the prevalence of the disorders that paroxetine treats.
Third, many specialties were found to be overrepresented in prescribing paroxetine, as indexed by ratios of the percent of paroxetine prescriptions to the percent of clinicians in Medicare who belong to that specialty.
MedicalResearch.com: What should readers take away from your report?
Response: It is encouraging that we observed a decreased population-corrected utilization of paroxetine, but it still was commonly used in this population despite explicit concern regarding the use of the medication in older adults. Paroxetine utilization is highly geographically variable, and more study is needed to explain this. Many specialties are overrepresented in paroxetine prescriptions, so specialty-specific approaches may not be the best approach to improve prescribing practices of paroxetine. Multiple possibilities could improve prescribing practices of paroxetine in older adults: integrating clinical pharmacists in medication reconciliation, routine review with standardized tools (e.g., Beers, STOPP/START), using computerized reminder systems, and increasing prescriber training in geriatric pharmacotherapy. 10–12
MedicalResearch.com: What further questions remain to be answered in this answer? What further research is indicated?
Response: This study’s findings require more research to better understand the reasoning for the observed findings. Namely, what are the causes for the large geographic variation? Further, the observed decline in paroxetine use could be due to the continued mixed recommendation of paroxetine particularly in older adults but could also be due to a general preference for other antidepressants.
Many other medications and prescribing practices increase the risk of adverse outcomes for older adults.8 Thus, future studies could explore the pharmacoepidemiology of other PIMs and the practice of polypharmacy with certain higher-risk medications. Along the same lines, it would be fruitful to see how these practices compare before and after the introduction of clinical tools, such as the Beers Criteria and STOPP/START Criteria.
Read the full study here:
Cavanah LR, Goldhirsh JL, Huey LY, Piper BJ. National patterns of paroxetine use among US Medicare patients from 2015–2020. Front Psychiatry. 2024;15. doi:10.3389/fpsyt.2024.1399493
References
- Gelenberg AJ, Freeman MP, Markowitz JC, et al. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. Published online 2010.
- Practice guideline for the treatment of patients with panic disorder. Published online January 2009. doi:10.1176/appi.books.9780890423363.51396
- American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Published online March 2013. doi:10.1176/appi.books.9780890423363.149114
- Stahl SM. Stahl’s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications. Cambridge University Press; 2021.
- Nevels RM, Gontkovsky ST, Williams BE. Paroxetine—the antidepressant from Hell? Probably not, but caution required. Psychopharmacol Bull. 2016;46(1):77-104. Accessed July 25, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5044489/
- The 2012 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society Updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616-631. doi:10.1111/j.1532-5415.2012.03923.x
- The 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
- 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052-2081. doi:10.1111/jgs.18372
- Administration on Aging. 2020 Profile of Older Americans.; 2021.
- Soumerai SB, McLaughlin TJ, Avorn J. Improving drug prescribing in primary care: A critical analysis of the experimental literature. Milbank Q. 2005;83(4):10.1111/j.1468-0009.2005.00435.x. doi:10.1111/j.1468-0009.2005.00435.x
- Amanda Hanora Lavan JO, Grady PFG. Appropriate prescribing in the elderly: Current perspectives. World J Pharmacol. 2015;4(2):193-209. doi:10.5497/wjp.v4.i2.193
- Stuhec M, Zorjan K. Clinical pharmacist interventions in ambulatory psychogeriatric patients with excessive polypharmacy. Sci Rep. 2022;12(1):11387. doi:10.1038/s41598-022-15657-x
- Cavanah LR, Goldhirsh JL, Huey LY, Piper BJ. National patterns of paroxetine use among US Medicare patients from 2015–2020. Front Psychiatry. 2024;15. doi:10.3389/fpsyt.2024.1399493
Editor’s note: Trade names for paroxetine include: Aropax, Paxil, Pexeva, Seroxat, Sereupin and Brisdelle,
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition.
Some links may be sponsored. Products are not endorsed.
Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on August 6, 2024 by Marie Benz MD FAAD
