04 Apr Respiratory Helmets Can Decrease Need for Intubation and Spread of COVID-19 Virus
MedicalResearch.com Interview with:

Aurika Savickaite
Aurika Savickaite RN
Adult Gerontology Acute Care Nurse Practitioner
Bulletproof Coach
University of Chicago Medicine
MedicalResearch.com: Would you briefly explain what is meant by helmet-based ventilation? How does it work?
Response: For patients in respiratory failure, noninvasive positive pressure ventilation (NIPPV) is usually delivered through a nasal mask or facemask. Many patients develop pain, discomfort – even claustrophobia — from using NIPPV systems. The transparent helmet was developed to improve the tolerance of noninvasive ventilation. It allows the patient to see, read, speak and drink without interrupting noninvasive positive-pressure ventilation (NPPV).
The helmet has a sealed connection and a soft collar that adheres to the neck which helps prevent the air leaks that are very common with nasal- or face masks. High positive end-expiratory pressure (PEEP) is vital in treating patients in respiratory failure and thanks to helmets “none to minimum air leak” system, PEEP can be set high (up to 25). NIPPV via a nasal- or full-face mask typically begins to show air leaks when the required pressure exceeds 15-20cm H2O.
MedicalResearch.com: Is it expensive? Available? Easy to use?

The noninvasive ventilation helmet is a transparent hood that covers the entire head of the patient and has a rubber collar neck seal.The University of Chicago Medicine
Response: Helmets cost about $150 to $165, and currently are available from two companies: Sea-Long and Amron. We are updating the list of manufacturers 24/7.
Link here: https://www.helmetbasedventilation.com/post/where-to-get-a-helmet-for-helmet-based-ventilation
The helmet is easy to use and can be applied by a respiratory therapist or a nurse (based on experience).
As noted on our website, new companies making helmets, but who are not ready to sell yet. That means that they are testing helmets and will be selling them soon. We get at least one to two calls daily from the USA manufacturers who want to start production. We guide them and connect them with professionals who know the process well and can expedite the production. Other world countries, including Brazil, Argentina, Israel, and Greece have contacted us and have been advised to start making the helmets. We share all the information that can help and encourage transparency.
MedicalResearch.com: For whom should it be used, ie as first line therapy?
Response: Helmets have been used for acute respiratory distress syndrome (ARDS) patients for many years in Europe, especially Italy. Studies show that 54 percent of ARDS patients avoided the need for intubation. When helmet based NIPPV was used – the ICU mortality rate was only 6 percent vs 54 percent for intubated patients.
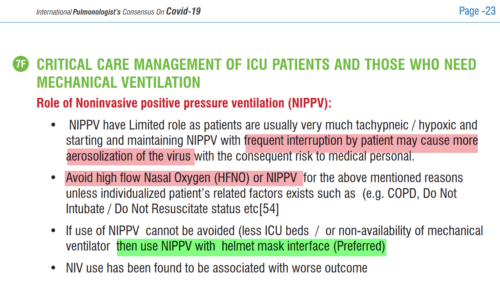
Today, based on international guidelines from pulmonologists around the world, helmets are preferred NIPPV for COVID-19 patients. The closed-airflow helmet system with a filter will prevent aerosolization of the virus and minimize the risk to medical personnel.
Based on feedback from Italian doctors, this therapy will prevent intubation for 20 to 30 percent of COVID-19 patients. In COVID19 intubated patients, the mortality rate is 70 to 86 percent.
MedicalResearch.com: Is there anything else you would like to add?
Response: With helmet NIPPV, the following issues can be resolved in the COVID19 pandemic:
- The shortage of ventilators: Helmets can be connected to oxygen with medical airflow or BiPAP machine.
- The shortage of medical staff and ICU rooms: Not all patients who are on NIPPV via helmet will need ICU rooms. Also, helmets are easy to manage and can be applied in a timely manner by respiratory therapists or nurses.
- Patients fail on prolonged NIPPV via nasal- or face mask and/or get intubated without trying NIPPV (guideline, vent shortages, etc): Helmets can be worn for a longer time and 20 to 30 percent of COVID-19 patients will avoid intubation. For many patients, symptoms will improve in the next one to two hours following helmet access and if no improvement is achieved, they will then get intubated.
Any disclosures?
HelmetBasedVentilation.com is a non-commercial private citizen initiative to organize information and help health care professionals learn the benefits of noninvasive ventilation (NIV) via the helmet. We publish information about the manufacturers, inventors and funding sources to help them connect so they can speed up the production of working helmets.
[wysija_form id=”3″]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on May 12, 2020 by Marie Benz MD FAAD