
18 Jun DCISionRT Tool Identifies DCIS Patients With High Risk of Recurrence After Surgery and Radiation
MedicalResearch.com Interview with:

Dr. Frank Vicini
Dr. Frank Vicini, MD, FACR, FASTRO
Principal Investigator
Radiation Oncologist at GenesisCare
Member of NRG Oncology
MedicalResearch.com: Would you briefly explain what is meant by DCIS?
Response: DCIS stands for ductal carcinoma in situ and indicates the presence of abnormal cells inside a milk duct in one or both breasts. Sometimes referred to as Stage 0 (zero), it is considered the earliest form of breast cancer and is noninvasive. The tumor has not yet left the duct– a passageway that transports milk from the breast lobules to the nipple– and begun to invade the healthy tissue surrounding it. Standard treatment options for DCIS include surgery, radiation therapy and hormonal therapy.
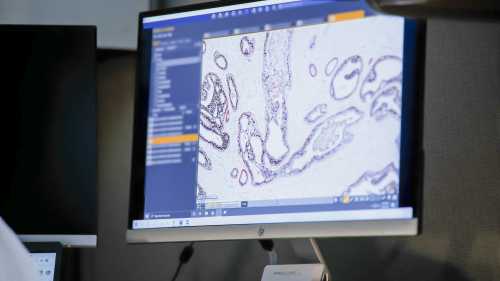
DCISionRT testing process includes advanced analysis of biomarker data from a DCIS patient’s specimen
MedicalResearch.com: Would you discuss the DCISionRT® testing and how it helps stratify patient risk?
Response: DCISionRT analyzes the biology of a patient’s unique tumor and provides a quantified risk of a woman’s cancer coming back within 10 years– either as invasive cancer or a DCIS recurrence– in the form of her Decision Score on a scale of zero to 10. Results also include specific percentages of how a patient’s risk changes based on the potential administration of radiation therapy after surgery versus surgery alone in order to equip her and her medical team with the most precise, personalized information when approaching treatment decisions.
MedicalResearch.com: What is the background for this study?
Response: PreludeDx potentially identified an unmet need in the breast cancer field to distinguish women diagnosed with DCIS who have a low risk of recurrence and are therefore potentially eligible to safely forgo radiation therapy after receiving breast conserving surgery (BCS) from those who have an elevated risk of recurrence even after both BCS and radiation therapy.
DCISionRt and its response subtype (Rst) biosignature were developed as a result and evaluated in a contemporary cohort of 485 women from US, Sweden and Australia who were treated with or without radiation therapy following BCS with negative margins in order to differentiate between these risk groups.
Patients were classified into Low and Elevated risk groups to assess the rates of DCIS recurrence, also known as ipsilateral breast tumor recurrence (IBTR), or Invasive Breast Cancer (IBC) development. Patients in the Elevated risk group were further categorized by good and poor Rst. Women in the good Rst risk group experienced exceptional RT benefit after BCS, where the poor Rst risk group experienced an unacceptable high rate of recurrence after BCS.
MedicalResearch.com: What are the main findings?
Response: In the Elevated risk group, radiation therapy was associated with significantly reduced recurrence rates, but only for those patients with a good Rst. Elevated risk patients with a poor Rst showed minimal benefit to radiation therapy and regardless of whether or not they received it, had 10-year IBTR/IBC of 25%/16% respectively compared to the good Rst rates of 6.6%/4.5%.
Patients in the Low risk group showed no significant difference in 10-year IBTR/IBC rates with radiation, 6.3%/2.7%, and without radiation, 4.1%/2.9%. Traditional clinicopathologic risk factors such as age (<50), grade (3) and tumor size (>2.5 cm) did not identify poor vs. good response subtypes. Multivariable analysis indicated that these factors and endocrine therapy were not significantly associated with IBTR or IBC.
MedicalResearch.com: What should readers take away from the DCISionRT report?
Response: DCIS is not a one-size-fits-all disease and should not be treated as such. Factoring in the patient’s biology allows for the development of a precise treatment approach tailored specifically to her genomics. DCISionRT test results arm physicians and patients with the information they need to make informed decisions and avoid the consequences of both over- and under-treatment by providing a quantified risk of recurrence based on surgery alone or surgery plus radiation.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: As a result of this study, further validation of the Rst biosignature in larger cohorts of patients are warranted and presently in progress. Additionally, studies examining intensified treatment modalities and corresponding patient outcomes for patients in the poor Rst risk group will also be valuable.
In this study, a subset of patients in the Elevated Risk group were HER2 3+; 38% had good Rst and 62% had poor Rst. Future research on the subset of these HER2 3+ patients warrant further investigation to gain insights on optimal treatment modalities as it appears only the patients with good Rst will respond optimally to standard treatment of BCS and RT.
Any disclosures?
Employment: Genesis Care
Consulting or advisory Role: Impedimed; PreludeDx
Citation: ASCO 21 abstract:
A Novel Biosignature Identified DCIS Patients with a Poor Biologic Subtype with Unacceptably High Rates of Local Recurrence after Breast Conserving Surgery and Radiotherapy
Link to Poster https://preludedx.com/wp-content/uploads/2021/05/2021-ASCO-Poster1.pdf
Link to website: www.preludedx.com
[subscribe]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on June 19, 2021 by Marie Benz MD FAAD
