20 Jul Italian Study Finds Patients’ Preferences Are Largely Ignored in Kidney Allocation Algorithms
MedicalResearch.com Interview with:

Dr. Pasini
Giacomo Pasini, PhD
Professor of Econometrics – Professore ordinario
Economics PhD program Director – Coordinatore dottorato in Economia
Rector’s delegate for Cooperation and Development – Delegato alla Cooperzione per lo sviluppo
Economics Department – Dipartimento di Economia
Universita’ Ca’ Foscari – Venezia
MedicalResearch.com: What is the background for this study?
Response: Kidney transplantation carries several advantages over dialysis treatment for patients with end-stage renal dis-ease (ESRD). Nevertheless, the disparity between the large number of transplant candidates and the scarcity of organs available continues to increase.
In order to close this gap selection criteria for donor appropriateness have been widened significantly in recent years to include older persons and those with co-morbidities that could potentially increase the risk of infectious disease transmission (the so-called Expanded Criteria Donors, ECD). The result of kidney transplantation from marginal donors is one of the most topical issues in the transplant literature.
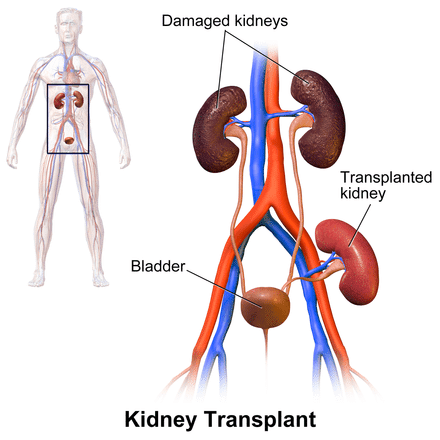
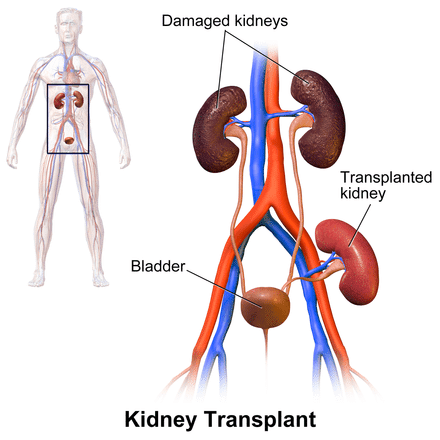
Kidney Transplant Wikipedia image
MedicalResearch.com: What are the main findings?
Response: From a clinical point of view, ECD or “marginal” kidneys, while inferior to standard criteria donor (SCD) kidneys, may prolong the life of the recipient compared to dialysis treatment. Moreover, transplantation with a marginal donor kidney is more cost-effective than dialysis as a means of treating ESRD
MedicalResearch.com: What should readers take away from your report?
Response: Patients’ preferences are largely ignored in kidney allocation algorithms. This is true for any organ transplant, but, while in the case of other organs (e.g., liver, heart, and lung) alternative options are considerably limited, dialysis could be a reasonable option against which patients on the waiting list can balance risks and benefits. We found a significant heterogeneity in the preferences of patients who are waiting for a transplant. Furthermore, we have proved how including patients’ preferences in the kidney allocation algorithm would considerably improve both the patients’ satisfaction and the expected graft survival. While marginal kidneys are currently offered only to those patients who have been on the waiting list for a long time, our article suggests there might be more patients who are willing to accept a marginal kidney right away.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: This paper suggests that a systematic and standardised patients’ preference elicitation could be a useful instrument to improve welfare in organ allocation mechanisms. The natural next step is to study how to maximize graft survival and patients’ satisfaction by means of allocation algorithms that account for preferences.
MedicalResearch.com: Is there anything else you would like to add?
Response: This project was supported by the “Progetto di Ateneo KIDNEY” from the University of Padua, and has been completed in collaboration with the team of surgeons of the Transplant Unit of the University of Padova Hospital, particularly Paolo Rigotti and Lucrezia Furian.
Citation:
The role of heterogeneity of patients’ preferences in kidney transplantation
Mesfin G.Genie Antonio Nicoló Giacomo Pasini
https://doi.org/10.1016/j.jhealeco.2020.102331
Journal of Health Economics
Volume 72, July 2020, 102331
JOIN OUR EMAIL LIST
[mailpoet_form id="5"]We respect your privacy and will never share your details.
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on July 20, 2020 by Marie Benz MD FAAD
