Author Interviews / 28.08.2020
Icahn Mt.Sinai Study Identifies Two Switches That Regulate RNA Transcription in Cancer Cells
MedicalResearch.com Interview with:
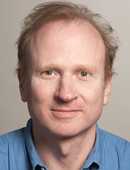
Robert Fisher, MD, PhD
Professor of Oncological Sciences
Icahn School of Medicine at Mount Sinai
Member of The Tisch Cancer Institute
MedicalResearch.com: What is the background for this study?
Response: Gene transcription by RNA polymerase II underlies cellular identity, and cell fate decisions such as proliferation or death, and is regulated by enzymes that add phosphates (kinases) or remove them (phosphatases) from components of the transcription machinery. Here we define two kinase-phosphatase switches that regulate different steps of the transcription cycle in human cancer cells.
We raised antibodies specific for different phosphorylated states of a key elongation factor, Spt5, and used genomic analyses such as chromatin immunoprecipitation and sequencing (ChIP-seq) to monitor when these phosphorylations were added and removed, and by which kinases and phosphatases, respectively, as RNA polymerase II traversed genes in human cancer cells. (more…)