Author Interviews, BMJ, Obstructive Sleep Apnea, Pediatrics, Sleep Disorders, Surgical Research / 09.11.2018
Tonsillectomy Often Done When Not Indicated (and vice versa!)
MedicalResearch.com Interview with:
Tom Marshall, MSc, PhD, MRCGP, FFPH
Professor of public health and primary care
Institute of Applied Health Research
University of Birmingham, Birmingham, UK
MedicalResearch.com: What is the background for this study?
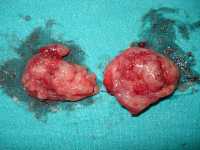
Response: Tonsillectomy is one of the most common childhood surgical procedures. There are two main indications: recurrent sore throat and sleep-related breathing problems (including obstructive sleep apnoea).
Jack Paradise’s 1984 study made clear tonsillectomy is modestly effective in children with frequent, severe sore throats: seven in one year, or five yearly in two successive years, or three yearly in three successive years. Sore throats must have symptoms: fever, pus seen on tonsils, lymphadenopathy or confirmed Streptococcal infection. With surgery, children average two sore throats in the next year, without surgery, three. Two years later there is no difference. Further research shows the benefits are too tiny to justify surgery in children with less frequent, less severe or undocumented sore throats. Subsequent randomised controlled trials have not changed the evidence. There isn’t enough good evidence to support surgery in children with obstructive sleep apnoea or sleep related breathing problems.
Tonsillectomy is not a trivial procedure, about 2% are readmitted with haemorrhage and about 1 in 40,000 dies. Childhood tonsillectomy is linked to risk of adult autoimmune diseases. It is important to be sure tonsillectomy is only undertaken in children where there are evidence-based indications.
(more…)