15 Nov Keyhole vs Open Surgery For Ruptured Abdominal Aortic Aneurysm
MedicalResearch.com Interview with:
Professor JT Powell PhD, MD, FRCPath
Faculty of Medicine,
Department of Surgery & CancerImperial College London
MedicalResearch.com: What is the background for this study?
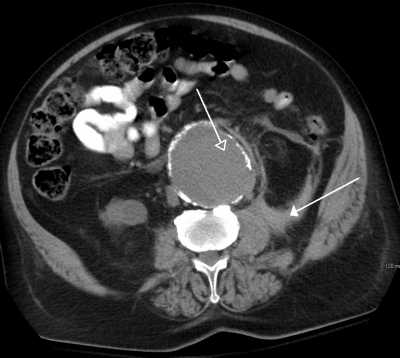
Response: The mortality from ruptured abdominal aortic aneurysm (AAA) remains very high causing about 6000 deaths each year in the UK. The only hope for survival is an emergency operation to repair the burst aorta. Even so the mortality may be as high as 45% within a month of repair using open surgery.
It has been suggested that minimally invasive repair using keyhole or endovascular techniques would lower the mortality to about 25% within a month of repair. However not all shapes of aorta are suitable for endovascular repair (also called EVAR).
MedicalResearch.com: What are the main findings?
Response: We established a multicentre randomised trial to compare a strategy of endovascular repair with open repair and followed up 613 patients for 3 years. Patients were recruited as soon as the diagnosis of rupture was made on clinical grounds (before diagnostic imaging) so that in the endovascular strategy group patients who were not suitable for EVAR (about one third of them) underwent open repair and some patients in each group died before repair. Disappointingly, at 1 month there was no difference in survival between the 2 randomised groups, each having a mortality of ~37%, although more patients were discharged directly to home from the endovascular strategy group and women had lower mortality in the endovascular strategy group.
In the following months quality of life was better in the endovascular strategy group and there was a similar rate of re-interventions between the randomised groups.
By 3 years, a survival advantage for the endovascular strategy group emerged, particularly for those who had actually received a repair for their rupture. For these latter patients, at 3 years survival in the endovascular strategy group was 58% versus only 46% in the open repair group and there was still no difference in the rate of re-interventions between the groups. Patients in the endovascular strategy group had gained an average of 0.17 quality-adjusted-life-years with less healthcare expenditure on aneurysm care. Therefore the endovascular strategy was both clinically effective and cost-effective.
MedicalResearch.com: What should clinicians and patients take away from your report?
Response: Based on these midterm results, there would appear to be a clear advantage for both patients and health providers for taking an endovascular strategy approach for ruptured AAA: endovascular repair whenever possible, with open repair as the default option. The reasons for the late emergence of a survival advantage for the endovascular strategy are not clearly defined but possibly relate to a reduced time spent in intensive care and a lower need for renal support.
MedicalResearch.com: What recommendations do you have for future research as a result of this study?
Response: Probably the main reason that there is no early advantage for the endovascular strategy is because the shock associated with AAA rupture kills the patient, irrespective of type of repair. We need further research about the best management of shock in these elderly patients and the options of using locoregional rather than general anaesthesia for emergency AAA repairs.
MedicalResearch.com: Is there anything else you would like to add?
Response: This research was funded by the National Institute of Health Research, UK and there are no disclosures. It has been a great team effort, since randomised trials in the life and death emergency setting are very challenging.
MedicalResearch.com: Thank you for your contribution to the MedicalResearch.com community.
Citation:
Note: Content is Not intended as medical advice. Please consult your health care provider regarding your specific medical condition and questions.
[wysija_form id=”1″]
Last Updated on November 15, 2017 by Marie Benz MD FAAD