15 Nov Breast Cancer: Risk-Adapted Starting Age of Screening for Relatives of Patients
MedicalResearch.com Interview with:
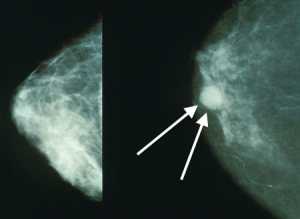
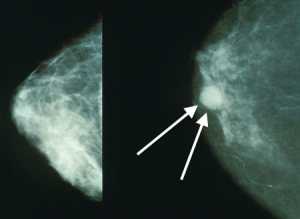
Mammograms showing a normal breast (left) and a breast with cancer (right, white arrows). Wikipedia Image
Dr. Elham Kharazmi, MD, PhD
Co-Leader, Risk Adapted Prevention (RAD) Group
Division of Preventive Oncology
National Center for Tumor Diseases (NCT)
German Cancer Research Center (DKFZ)
Germany
MedicalResearch.com: What is the background for this study?
Response: Breast cancer is the most common cancer in women worldwide and the second leading cause of cancer death in American women, exceeded only by lung cancer. Available evidence suggests that implementation of a screening program can decrease breast cancer mortality.
Reductions in breast cancer mortality in Europe over the past two decades have been associated at least in part with the implementation of screening programs. Screening enables the detection of tumors at an early stage, when more treatment options are feasible and most effective. However, screening is associated with substantial risks, such as over-diagnosis, false-positive results, and physical and psychological harms, particularly when large numbers of women with low risk are frequently screened.
Many national screening programs have adopted a one size-fits-all approach, advising women aged 50 to 69 years to obtain a biennial mammogram. Similarly, most breast cancer screening guidelines recommend a general starting age for screening for all women, even those at increased risk, such as those with family history of breast cancer. Family history is a non-modifiable risk factor for this cancer. Breast cancer risk associated with family history varies with age of the individual, nature and number of affected relatives, and age at which the relative received a diagnosis. Existing guidelines for women at increased risk, such as the American Cancer Society guidelines that recommend initiation of breast cancer screening at age 40 years or 10 years earlier than the youngest relative with a diagnosis, are largely based on expert opinion rather than empirical evidence.
Because age-oriented screening suggestions pay limited attention to individual risks based on known risk factors, the approach is considered suboptimal, and personalized screening has been advocated. Although many risk assessment models and tools have been developed so far, none of them provide the evidence-based risk-adapted starting age of screening for women with different constellations of family history.
MedicalResearch.com: What are the main findings?
Response: Our study used, to our knowledge, the world’s largest family-cancer datasets to assess the absolute familial risks associated with the age at diagnosis and number of first-degree and second-degree relatives. The goal was to establish a risk-adapted starting age of breast cancer screening based on these factors.
We found that risk-adapted starting age of breast cancer screening varied by the number of affected first- or second-degree relatives and by age at diagnosis of first-degree relatives. For example, when mass screening was recommended at age 50 years, women with multiple affected first-degree relatives reached the screening risk level at age 27 to 36 years, depending on the youngest age at diagnosis in relatives.
MedicalResearch.com: What should readers take away from your report?
Response: This study identifies risk-adapted starting ages for breast cancer screening based on detailed family history of breast cancer that can provide guidance to clinicians and relatives of patients with breast cancer on when to start timely screening. I would be happy to interpret personalized risk-adapted starting age of breast cancer screening for relatives of patients with breast cancer based on findings of this study. Interested person can contact me at elham.kharazmi@med.lu.se.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: We did not have data on other breast cancer risk factors, such as predisposing genes (eg, BRCA1, BRCA2, and PALB2) and mammographic breast density. In general, women with other known risk factors, such as cancer predisposing genes, are advised to start screening as recommended by guidelines for women with high risk if the guidelines offer an earlier starting age of screening than our familial risk-adapted starting age of screening. Further research incorporating all known risk factors of breast cancer for the optimal risk-adapted starting age of screening for breast cancer is warranted.
Citation:
Mukama T, Kharazmi E, Xing X, et al. Risk-Adapted Starting Age of Screening for Relatives of Patients With Breast Cancer. JAMA Oncol. Published online November 14, 2019. doi:https://doi.org/10.1001/jamaoncol.2019.3876
JOIN OUR EMAIL LIST
[mailpoet_form id="5"]We respect your privacy and will never share your details.
Last Modified: [last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on November 15, 2019 by Marie Benz MD FAAD
