Author Interviews, Breast Cancer, Mammograms / 07.12.2022
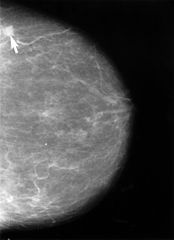
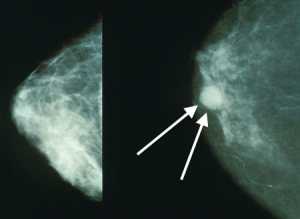
Contrast-enhanced mammography significantly improved detection of early breast cancer in women with Personal History of Breast Cancer
MedicalResearch.com Interview with:
Wendie Berg, MD, PhD, FACR
Professor of Radiology
University of Pittsburgh
MedicalResearch.com: What is the background for this study?
Response: Mammography misses many cancers in women with a personal history of breast cancer (PHBC). MRI improves early detection of cancer in women with PHBC and the American College of Radiology recommends adding MRI every year for women with PHBC and dense breasts or diagnosis by age 50 but not every woman can tolerate MRI.
Contrast-enhanced mammography (CEM) appears to be a good alternative to MRI. Our study examined performance of CEM after tomosynthesis in women with PHBC. We first trained our radiologists in CEM (Berg WA et al JBI 2021) and two radiologists interpreted both tomosynthesis and CEM on every participant.
(more…)