After Age 75 Mammograms May Not Decrease Chance of Dying of Breast Cancer
Awareness of Breast Density Importance Varies by State Laws and Social Factors
Morbidity of Breast Cancer and Screening Interval: Annual versus Biennial
Breast Cancer: Risk-Adapted Starting Age of Screening for Relatives of Patients
 Philippe Henrot, MD
Radiology Department
Institut de Cancerologie de Lorraine
Vandoeuvre-les-Nancy
MedicalResearch.com: What is the background for this study? What are the main findings?
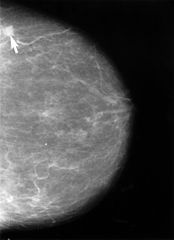
Response: The initial observation was that daily practice of mammography shows a substantial proportion of women that report a negative experience after having a mammogram. Compression of the breast before delivering X-rays is mandatory to achieve the best image quality and to detect small cancers. Unfortunately, compression is uncomfortable, even sometimes painful.
We took into consideration a study of PJ Kornguth et al. published in 1993 reporting the self-compression technique. In this study one breast was compressed by the radiographer and the other with self-compression. The author reported a high level of patient satisfaction, and a lower discomfort, without compromising image quality. We performed a multicenter prospective randomized trial to demonstrate the feasibility of the self-compression technique in condition similar to routine screening or follow-up, compared with standard compression. The primary outcome was to demonstrate that self-compression did not lead to compress the breast less than standard compression, and that was done. The secondary outcomes were to evaluate pain, compression force and image quality.
The results indicated that compression force was higher when the women controlled themselves the compression of their breast, and the pain measured on a visual analogue scale was lower. Moreover, image quality was not compromised compared with standard compression. (more…)
Philippe Henrot, MD
Radiology Department
Institut de Cancerologie de Lorraine
Vandoeuvre-les-Nancy
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The initial observation was that daily practice of mammography shows a substantial proportion of women that report a negative experience after having a mammogram. Compression of the breast before delivering X-rays is mandatory to achieve the best image quality and to detect small cancers. Unfortunately, compression is uncomfortable, even sometimes painful.
We took into consideration a study of PJ Kornguth et al. published in 1993 reporting the self-compression technique. In this study one breast was compressed by the radiographer and the other with self-compression. The author reported a high level of patient satisfaction, and a lower discomfort, without compromising image quality. We performed a multicenter prospective randomized trial to demonstrate the feasibility of the self-compression technique in condition similar to routine screening or follow-up, compared with standard compression. The primary outcome was to demonstrate that self-compression did not lead to compress the breast less than standard compression, and that was done. The secondary outcomes were to evaluate pain, compression force and image quality.
The results indicated that compression force was higher when the women controlled themselves the compression of their breast, and the pain measured on a visual analogue scale was lower. Moreover, image quality was not compromised compared with standard compression. (more…)Mammograms: Minorities and Poor Less Likely To Report Barriers to Care
Routine Mammography Screening Recommendations Do Not Apply To Women With History of Breast Cancer
Effects of Breast Density Notification Laws Vary By State
Targeting Breast Cancer Screening To Higher Risk Patients Reduces Overdiagnosis, Costs and Side Effects
MedicalResearch.com Interview with:
Dr Nora Pashayan PhD
Clinical Reader in Applied Health Research
University College London
Dept of Applied Health Research
London
MedicalResearch.com: What is the background for this study?
Response: Not all women have the same risk of developing breast cancer and not all women have the same potential to benefit from screening.
If the screening programme takes into account the individual variation in risk, then evidence from different studies indicate that this could improve the efficiency of the screening programme. However, questions remain on what is the best risk-stratified screening strategy, does risk-stratified screening add value for money, and what are benefit and harm trade-offs.
(more…)Mammograms Reduce Mortality From Higher Grade Breast Cancers
Stephen W. Duffy Professor of Cancer Screening Wolfson Institute of Preventive Medicine, Barts and The London School of Medicine and Dentistry Queen Mary University of London
MedicalResearch.com: What is the background for this study? What are the main findings? Response: The phenomenon of length bias, whereby screening has more chance of detecting slow growing tumours, has been known about for some years. This has led some colleagues to speculate that breast cancer screening only benefits those with slow-growing, less aggressive cancers, and does not reduce deaths from more aggressive, rapidly progressing cancers. In this study, we addressed this question directly using data from a randomised trial of mammographic screening. We calculated the reduction in mortality from grade 1 (less aggressive), grade 2 (intermediate) and grade 3 (most aggressive) cancers, as a result of screening. We found that the greatest reduction in breast cancer mortality was from the aggressive, fast-growing grade 3 cancers, contrary to what had been suspected. (more…)Machine Learning Applied To Predicting High-Risk Breast Lesions May Reduce Unnecessary Surgeries
No Magic Age To Stop Performing Screening Mammograms
False Positive Mammograms Can Lead Women To Delay or Skip Next Exam
How Can Radiologists Detect Cancer In a Fraction of a Second?
Breast Density Interpretation Varies Among Radiologists
 Brian L. Sprague, PhD
Assistant Professor
Department of Surgery
Assistant Professor
Department of Biochemistry
University of Vermont
MedicalResearch.com: What is the background for this study?
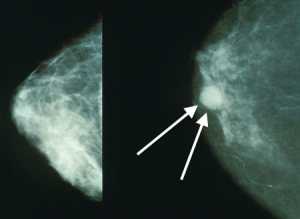
Response: Having dense breasts makes mammography more difficult to interpret and is also an independent risk factor for developing breast cancer. About half of all U.S. states require that information on the density of a woman's breasts be made available to her after a mammogram, and in some states the report must also inform such women that there are additional tests, such as breast magnetic resonance imaging (MRI), that may detect breast cancer in women who have dense breasts and normal mammograms.
Such laws are controversial because of the large number of women affected (around 40% of women aged 40-74) and due to a lack of consensus in the medical community regarding the benefits and harms of supplemental screening strategies. An additional concern is the subjective nature of breast density assessment, which is based on the Breast Imaging Reporting and Data System (BI-RADS) that provides four possible categories for breast density.
(more…)
Brian L. Sprague, PhD
Assistant Professor
Department of Surgery
Assistant Professor
Department of Biochemistry
University of Vermont
MedicalResearch.com: What is the background for this study?
Response: Having dense breasts makes mammography more difficult to interpret and is also an independent risk factor for developing breast cancer. About half of all U.S. states require that information on the density of a woman's breasts be made available to her after a mammogram, and in some states the report must also inform such women that there are additional tests, such as breast magnetic resonance imaging (MRI), that may detect breast cancer in women who have dense breasts and normal mammograms.
Such laws are controversial because of the large number of women affected (around 40% of women aged 40-74) and due to a lack of consensus in the medical community regarding the benefits and harms of supplemental screening strategies. An additional concern is the subjective nature of breast density assessment, which is based on the Breast Imaging Reporting and Data System (BI-RADS) that provides four possible categories for breast density.
(more…)GW Radiologist Discusses Implications of Breast Density Notification Laws
Performance of Mammogram Readers Does Not Diminish With Time
New Breast Cancer Screening Recommendations Carry Risks Of Later Diagnosis
Study Finds Regular Mammography May Provide Benefit Up To Age 84
Ultrasonography For All Dense Breasts Not Cost Effective
 MedicalResearch.com Interview with:
Brian L. Sprague, PhD
Office of Health Promotion Research,
University of Vermont, Burlington, VT
MedicalResearch: What is the background for this study?
Dr. Sprague: Mammographic breast density refers to the appearance of breast tissue on a mammogram. High breast density means that there is a greater amount of glandular tissue and connective tissue, which appears white on a mammogram. It is more difficult to detect breast cancer on a mammogram when there is greater breast density. It has also been shown that women with dense breasts are at a higher risk of developing breast cancer. Because of these two factors, women with dense breasts have a greater chance of developing breast cancer after a normal screening mammogram than women whose breasts are not dense. Many states have now passed laws that require mammography facilities to inform women with dense breasts so that they are aware of this. Similar legislation is now under consideration at the national level. More than 40% of women undergoing mammography screening have dense breasts.
Researchers are trying to determine whether supplemental breast cancer screening with other tools would improve outcomes for women with dense breasts. One possible approach is to use ultrasound imaging to screen for breast cancer in women with dense breasts after they have had a normal mammogram. We wanted to estimate the benefits, harms, and cost-effectiveness of this approach compared to mammography screening only. No randomized trials or observational studies have assessed long term outcomes after ultrasound screening for women with dense breasts, but we have short term data on how often cancer is diagnosed by ultrasound screening and how often false positive exams occur. We used computer simulation modeling to estimate long term outcomes by combining the currently available data on mammography and ultrasound screening with the best available data on breast cancer risk and survival.
(more…)
MedicalResearch.com Interview with:
Brian L. Sprague, PhD
Office of Health Promotion Research,
University of Vermont, Burlington, VT
MedicalResearch: What is the background for this study?
Dr. Sprague: Mammographic breast density refers to the appearance of breast tissue on a mammogram. High breast density means that there is a greater amount of glandular tissue and connective tissue, which appears white on a mammogram. It is more difficult to detect breast cancer on a mammogram when there is greater breast density. It has also been shown that women with dense breasts are at a higher risk of developing breast cancer. Because of these two factors, women with dense breasts have a greater chance of developing breast cancer after a normal screening mammogram than women whose breasts are not dense. Many states have now passed laws that require mammography facilities to inform women with dense breasts so that they are aware of this. Similar legislation is now under consideration at the national level. More than 40% of women undergoing mammography screening have dense breasts.
Researchers are trying to determine whether supplemental breast cancer screening with other tools would improve outcomes for women with dense breasts. One possible approach is to use ultrasound imaging to screen for breast cancer in women with dense breasts after they have had a normal mammogram. We wanted to estimate the benefits, harms, and cost-effectiveness of this approach compared to mammography screening only. No randomized trials or observational studies have assessed long term outcomes after ultrasound screening for women with dense breasts, but we have short term data on how often cancer is diagnosed by ultrasound screening and how often false positive exams occur. We used computer simulation modeling to estimate long term outcomes by combining the currently available data on mammography and ultrasound screening with the best available data on breast cancer risk and survival.
(more…)Risk-Based Mammography Recommendations May Miss Some Breast Cancers
 MedicalResearch.com Interview with:
Elissa R. Price, MD
Assistant Professor of Clinical Radiology
Director of Clinical Operations, Breast Imaging
Breast Imaging Fellowship Program Director
Department of Radiology and Biomedical Imaging
University of California, San Francisco San Francisco, CA 94115
MedicalResearch: What is the background for this study? What are the main findings?
Dr. Price: Screening mammography recommendations for the 40 - 49 age group is very controversial. 2009 USPTF guidelines emphasized taking patient context into account when making decisions for these young women. Recent publications have suggested risk-based screening strategies. Family history and breast density are important are easily accessible risk factors.
Had we been using this risk-based approach to screening mammography at our institution, we would have missed more than 3Ž4 of the screen detected breast cancers in the 40-49 age group, thereby foregoing most of the survival benefit from screening mammography.
(more…)
MedicalResearch.com Interview with:
Elissa R. Price, MD
Assistant Professor of Clinical Radiology
Director of Clinical Operations, Breast Imaging
Breast Imaging Fellowship Program Director
Department of Radiology and Biomedical Imaging
University of California, San Francisco San Francisco, CA 94115
MedicalResearch: What is the background for this study? What are the main findings?
Dr. Price: Screening mammography recommendations for the 40 - 49 age group is very controversial. 2009 USPTF guidelines emphasized taking patient context into account when making decisions for these young women. Recent publications have suggested risk-based screening strategies. Family history and breast density are important are easily accessible risk factors.
Had we been using this risk-based approach to screening mammography at our institution, we would have missed more than 3Ž4 of the screen detected breast cancers in the 40-49 age group, thereby foregoing most of the survival benefit from screening mammography.
(more…)Study Finds Breast Cancer Screening Should Begin Around Age 40
 MedicalResearch.com Interview with:
Blake Cady MD
Professor of Surgery (emeritus) at Harvard Medical School
Partners HealthCare, Harvard Medical
School institutions, Boston
Medical Research: What are the main findings of this study?
Dr. Cady: Our findings support mammography screening, and our data is consistent
with the randomized trials. Breast cancer screening with mammography is the most extensively researched screening method ever studied. Only one “randomized" trial failed to show reduced mortality, (Canadian NCSS studies), and there were major flaws in its design and execution that negate their results, as noted in multiple critical publications (volunteers, not geographic assignment, palpable masses detected at examination assigned to “screening” arm, large contamination bias (control group got screened anyway), and very poor quality of mammography). Yet it is this NCSS study that is cited by critics and the press. “Failure Analyses” look backward from death, rather than forward from assignment in randomized trials. The concept of failure studies is well established as noted in recent reports of air-bag failures in cars, and many industrial studies. Seat belt prevention of deaths was discovered by police recording injuries and deaths in crashes after the fact - a failure analysis - not by randomized clinical trials. In breast cancer, failure analyses have advantages of little cost, early results, simplicity, and convenience, compared to randomized trials. Since our results support findings from randomized clinical trials (RCT), they can be accepted as reliable and accurate.
Our findings show that about 71% of deaths from breast cancer occur in the approximately 20% of our patients not in regular screening programs, while only 29% of deaths occur in the 80% of women who were regularly screened by mammography. By extrapolation, women regularly screened have only about a 5% breast cancer mortality, but women not screened have close to a 50% mortality.
(This is my extrapolation from our data, not direct data from our “Failure Analysis”)
(more…)
MedicalResearch.com Interview with:
Blake Cady MD
Professor of Surgery (emeritus) at Harvard Medical School
Partners HealthCare, Harvard Medical
School institutions, Boston
Medical Research: What are the main findings of this study?
Dr. Cady: Our findings support mammography screening, and our data is consistent
with the randomized trials. Breast cancer screening with mammography is the most extensively researched screening method ever studied. Only one “randomized" trial failed to show reduced mortality, (Canadian NCSS studies), and there were major flaws in its design and execution that negate their results, as noted in multiple critical publications (volunteers, not geographic assignment, palpable masses detected at examination assigned to “screening” arm, large contamination bias (control group got screened anyway), and very poor quality of mammography). Yet it is this NCSS study that is cited by critics and the press. “Failure Analyses” look backward from death, rather than forward from assignment in randomized trials. The concept of failure studies is well established as noted in recent reports of air-bag failures in cars, and many industrial studies. Seat belt prevention of deaths was discovered by police recording injuries and deaths in crashes after the fact - a failure analysis - not by randomized clinical trials. In breast cancer, failure analyses have advantages of little cost, early results, simplicity, and convenience, compared to randomized trials. Since our results support findings from randomized clinical trials (RCT), they can be accepted as reliable and accurate.
Our findings show that about 71% of deaths from breast cancer occur in the approximately 20% of our patients not in regular screening programs, while only 29% of deaths occur in the 80% of women who were regularly screened by mammography. By extrapolation, women regularly screened have only about a 5% breast cancer mortality, but women not screened have close to a 50% mortality.
(This is my extrapolation from our data, not direct data from our “Failure Analysis”)
(more…)Annual Mammograms Did Not Save Lives in 25 Year Study
 MedicalResearch.com Interview with:
Anthony Miller, MD
Director, Canadian National Breast Screening Study
Professor Emeritus, Dalla Lana School of Public Health
University of Toronto
MedicalResearch.com: What are the main findings of the study?
Prof. Miller: The study involved 89,835 women aged 40 to 59. All underwent an annual physical breast examination, while half were randomly assigned to undergo annual mammograms for five years, beginning in 1980.
During the five-year screening period, 666 invasive breast cancers were diagnosed in the mammography arm and 524 in the controls. Over the 25 year follow-up 180 women in the mammography arm and 171 women in the control arm died of breast cancer. The overall hazard ratio for death from breast cancer diagnosed during the screening period associated with mammography was 1.05 (95% CI: 0.85 – 1.30). The findings for women aged 40-49 and aged 50-59 were almost identical.
After 15 years of follow-up an excess of 106 cancers was observed in the mammography arm, attributable to over-diagnosis, i.e. 22% of screen-detected invasive breast cancers, half of those detected by mammography alone. This represents one over-diagnosed breast cancer for every 424 women screened by mammography.
By 2005, 3,250 of the 44,925 women in the mammography arm of the study were diagnosed with breast cancer, and 500 had died of it. The control group of 44,910 women had 3,133 breast cancer diagnoses and 505 breast cancer deaths.
We conclude that annual mammography in women aged 40-59 does not reduce mortality from breast cancer beyond that of physical examination or usual care when adjuvant therapy for breast cancer is freely available.
(more…)
MedicalResearch.com Interview with:
Anthony Miller, MD
Director, Canadian National Breast Screening Study
Professor Emeritus, Dalla Lana School of Public Health
University of Toronto
MedicalResearch.com: What are the main findings of the study?
Prof. Miller: The study involved 89,835 women aged 40 to 59. All underwent an annual physical breast examination, while half were randomly assigned to undergo annual mammograms for five years, beginning in 1980.
During the five-year screening period, 666 invasive breast cancers were diagnosed in the mammography arm and 524 in the controls. Over the 25 year follow-up 180 women in the mammography arm and 171 women in the control arm died of breast cancer. The overall hazard ratio for death from breast cancer diagnosed during the screening period associated with mammography was 1.05 (95% CI: 0.85 – 1.30). The findings for women aged 40-49 and aged 50-59 were almost identical.
After 15 years of follow-up an excess of 106 cancers was observed in the mammography arm, attributable to over-diagnosis, i.e. 22% of screen-detected invasive breast cancers, half of those detected by mammography alone. This represents one over-diagnosed breast cancer for every 424 women screened by mammography.
By 2005, 3,250 of the 44,925 women in the mammography arm of the study were diagnosed with breast cancer, and 500 had died of it. The control group of 44,910 women had 3,133 breast cancer diagnoses and 505 breast cancer deaths.
We conclude that annual mammography in women aged 40-59 does not reduce mortality from breast cancer beyond that of physical examination or usual care when adjuvant therapy for breast cancer is freely available.
(more…)