05 Dec Prions of Creutzfeldt-Jakob Disease Detected Throughout Eye Tissues
MedicalResearch.com Interview with:
 Byron Caughey, Ph.D.
Byron Caughey, Ph.D.
Senior Investigator
Chief, TSE/prion Biochemistry Section
Laboratory of Persistent Viral Diseases
NIH/NIAID Rocky Mountain Laboratories
Hamilton, MT 59840 USA
MedicalResearch.com: What is the background for this study? What are the main findings?
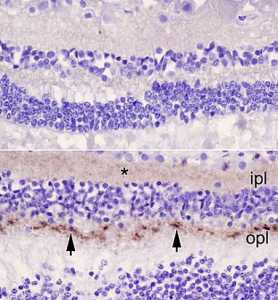
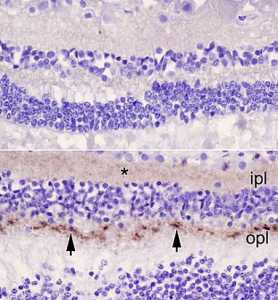
Response: Corneal transplants have caused the transmission of Creutzfeldt-Jakob disease (CJD) in at least two cases, and pathological prion protein has been detected in the retinas of the eyes of sporadic CJD cases. To build on these previous indications of prions in eye tissue, we tested the distribution of prions in various components of eyes from 11 sCJD decedents.
We applied a highly sensitive surrogate test for prions (RT-QuIC) that indicated that all of the sCJD cases had prions in multiple parts of their eye, including the cornea and sclera, which is the white outer surface of the eye. Retinas were usually contained the highest levels, in some cases approaching levels in the brain. Some other parts such as the cornea, lens and vitreous had much lower, but detectable, levels.
MedicalResearch.com: What should readers take away from your report?
Response: Our ability to detect prions in multiple eye components might aid antemortem diagnostic testing for prion disease. Also, our results augment concerns that such ocular prions might present risks of transmission via medical procedures involving the eye.
However, I know of no evidence that routine eye exams, or casual interactions involving contact with the eye, have transmitted Creutzfeldt-Jakob disease .
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Given these possible risks (albeit presumably low), ophthalmologists might consider using disposable instruments that contact the eye whenever feasible, or using effective anti-prion decontamination treatment on instruments that are reused.
MedicalResearch.com: Is there anything else you would like to add?
Response: The approach that we have described might also be applicable to the detection of other putatively prion-like misfolded protein aggregates in eye tissue. For example, we have developed similar highly sensitive RT-QuIC tests for the aggregated proteins that cause Parkinson’s disease, Alzheimer’s disease and some other neurodegenerative diseases and plan to apply them to eye tissue from relevant cases.
Disclosures: Some coauthors of this study are named as inventors of RT-QuIC technologies that relate to these studies.
Citation:
References:Prion Seeds Distribute throughout the Eyes of Sporadic Creutzfeldt-Jakob Disease Patients. Orrù CD, Soldau K, Cordano C, Llibre-Guerra J, Green AJ, Sanchez H, Groveman BR, Edland SD, Safar JG, Lin JH, Caughey B, Geschwind MD, Sigurdson CJ. MBio. 2018 Nov 20;9(6). pii: e02095-18. doi: 10.1128/mBio.02095-18. PMID: 30459197.
Funding:NIH’s Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Neurological Disorders and Stroke (NINDS), and National Institute on Aging; Michael J. Homer Family Fund; Equity in Brain Health at the Global Brain Health Institute; and donations to the NIAID Gift Fund from Mary Hilderman Smith, Zoë Smith Jaye, and Jenny Smith Unruh in memory of Jeffrey Smith.
[wysija_form id=”3″]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on December 5, 2018 by Marie Benz MD FAAD
