Author Interviews, COVID -19 Coronavirus, Critical Care - Intensive Care - ICUs, Pulmonary Disease / 15.01.2021
Rapid Test Identifies Secondary Pneumonia infections in COVID-19 Patients
MedicalResearch.com Interview with:
Dr Andrew Conway Morris
Wellcome Trust Clinical Research Career Development Fellow
University of Cambridge
Hon Consultant in Intensive Care Medicine
Addenbrookes Hospital, Cambridge
MedicalResearch.com: What is the background for this study?
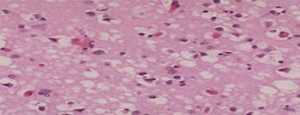
Response: Patients with COVID-19 frequently need to come to the intensive care unit (ICU), where we use mechanical ventilation to support their lungs as they get over the intense inflammation caused by the virus. During the first wave of the virus we noted that a lot of our patients appeared to be developing secondary infections (infections they didn’t have when they came into the ICU).
We therefore rolled out a rapid diagnostic test for these secondary bacterial infections that we had developed previously, and this study reports the use of this diagnostic and also describes the types of bacteria seen. To see if the increase in secondary infections was due to COVID specifically, we compared them to patients who were managed in the same ICU but who did not have COVID.
(more…)