MedicalResearch.com Interview with:
Sheila Connelly, PhD
Vice President, Research
Synthetic Biologics, Inc.
MedicalResearch.com: What is the background for this study?
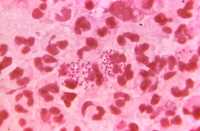
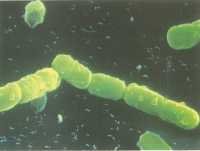
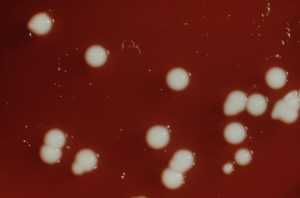
Response: Synthetic Biologics, Inc. is focused on the protection and preservation of the gut microbiome which is the diverse collection of microorganisms that live in the intestinal tract. We are learning that the gut microbiome plays a key role in health. Negative changes to the microbiome, called dysbiosis, are linked to disease states including allergies, autism, and obesity, among a rapidly growing list of other conditions. A consequence of using antibiotics is that, in addition to fighting the bacterial infection being treated, they also kill the gut microbiota. The space left in the gut by the dead bacteria allows other surviving bacteria, many times opportunistic pathogens or microbes that are resistant to multiple antibiotics, to overgrow and fill the open niches. Exposure to antibiotics, particularly broad-spectrum antimicrobials, such as penicillins and cephalosporins, is a major risk factor for acquiring a potentially deadly
Clostridium difficile infection.
Another consequence of antibiotic use is the emergence of antibiotic-resistant organisms. Widespread use of antibiotics provides selective pressure for the evolution of lethal, multi-drug resistant pathogens, termed “nightmare bacteria”. The gut microbiome acts as a reservoir of antibiotic resistance that can be triggered, by antibiotic exposure, to acquire and propagate resistance genes.
A way to protect the microbiome and reduce antibiotic resistance is to limit exposure of the gut microbiota to antibiotics. To this end, we developed an antibiotic inactivation strategy using a beta-lactamase enzyme to degrade beta-lactam antibiotics in the GI tract before they can harm the gut microbiome. Beta-lactamases are naturally-occurring bacterial enzymes that confer resistance to beta-lactams, the most widely used broad spectrum antibiotics, and their presence is normally considered an obstacle to efficacious infection control. We took advantage of the highly efficient antibiotic degradation activity of a beta-lactamase and developed SYN-004 (ribaxamase). Ribaxamase is a beta-lactamase engineered to inactivate penicillins and most cephalosporins, formulated for oral delivery, and intended for use with IV beta-lactam antibiotics to degrade the antibiotics in the GI tract to protect the microbiome.
Ribaxamase was demonstrated to significantly reduce the occurrence of
C. difficile disease in a recently completed Phase 2b clinical study. The study met its primary endpoint by demonstrating that ribaxamase, when delivered orally with IV ceftriaxone, significantly reduced
C. difficile disease in patients treated for a respiratory tract infection. Ribaxamase also resulted in a significant reduction in new colonization by vancomycin-resistant enterococcus (VRE).
For the current study, pig models of antibiotic-mediated gut dysbiosis were established using three classes of beta-lactam antibiotics, a cephalosporin, ceftriaxone, a penicillin, amoxicillin, and a carbapenem, ertapenem. The ceftriaxone model was used to evaluate the protective effect of ribaxamase on the microbiome and the amoxicillin and ertapenem models are intended for evaluation of pipeline products.
(more…)