Author Interviews, Emory, Infections, JAMA, MRSA / 10.10.2023
Emory/CDC Study Finds Combination Strategy Reduces Hospital Acquired Staph Infections
MedicalResearch.com Interview with:
Dr. John Jernigan, MD MS
Clinical Associate Professor of Medicine
Division of Infectious Diseases
Emory University School of Medicine
Branch Chief
Epidemiology, Research and Innovations Branch
CDC Center for Disease Control
MedicalResearch.com: What is the background for this study?
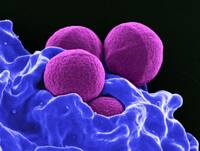
Response: Staphylococcus aureus commonly causes infections in ICUs. One approach to preventing these infections is using nasal mupirocin plus chlorhexidine gluconate (CHG) bathing for ICU patients. This practice is known to prevent methicillin-resistant Staphylococcus aureus (MRSA) infections and all-cause. bloodstream infections. This practice has been broadly adopted in ICUs in the US, but adoption of mupirocin as a universal topical antibiotic has been slowed by concerns for engendering mupirocin resistance.
This cluster-randomized trial in adult ICUs was conducted to assess whether universal nasal antiseptic povidone-iodine (iodophor), to which minimal S. aureus resistance is expected, was an acceptable alternative to universal nasal mupirocin for reducing S. aureus and MRSA clinical cultures in the setting of daily CHG bathing. Those who received chlorhexidine (CHG) bathing with mupirocin had an 18% reduction in risk of Staphylococcus aureus clinical cultures and a 15% reduction in risk of methicillin-resistant S. aureus (MRSA) clinical cultures compared to patients who received CHG bathing with intranasal iodophor. These results show that using mupirocin for nasal decolonization may be preferred over iodophor because it is more effective at preventing S. aureus infections.
(more…)