Author Interviews, Heart Disease, JACC / 10.04.2019
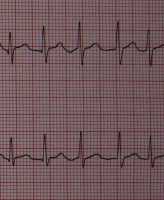
Collagen Biomarker Associated With Atrial Fibrillation and Heart Failure Risk
MedicalResearch.com Interview with:
Susana Ravassa PhD
Program of Cardiovascular Diseases, CIMA
University of Navarra, and IdiSNA
Navarra Institute for Health Research
Pamplona, Spain
MedicalResearch.com: What is the background for this study?
Response: Atrial fibrillation (AF) is an evolving epidemic responsible for substantial morbidity, mortality and health-care expenditure. In particular, when AF and heart failure (HF) occur in combination, clinical evolution is particularly poor. Left atrial (LA) myocardial interstitial fibrosis (MIF) is the main structural lesion in AF and considered as the main factor responsible for the perpetuation of this pathology. In addition, it is known that MIF is associated with a lower effectiveness of the treatment of AF by pulmonary vein isolation with catheter ablation. Therefore, the identification of biomarkers related to MIF, as an affordable and minimally invasive approach, is of great interest to detect patients at risk of AF, as well as to monitor their response to the LA ablation therapy.
We had previously demonstrated that the deleterious impact of MIF in the heart is due to alterations in both the quality (i.e., extent of cross-linking among collagen fibrils and type of collagen fibers that determine their rigidity and resistance to degradation [collagen cross-linking or CCL]) and the quantity (i.e., extent of collagen fibers that occupy the myocardial tissue [collagen deposition or CD]) of fibrotic tissue. We have shown that certain circulating biomarkers related to collagen type I metabolism are associated with CCL and CD. On the one hand, the serum carboxy-terminal propeptide of procollagen type I (PICP), released during the conversion of procollagen type I into fibril-forming mature collagen type I, is directly correlated with myocardial CD.
On the other hand, the ratio of serum carboxy-terminal telopeptide of collagen type I to serum matrix metalloproteinase-1 (serum CITP:MMP-1 ratio) is inversely correlated with myocardial CCL, as the higher is the cross-linking among collagen type I fibrils the lower will be the cleavage of CITP by MMP-1 during the process of degradation of the fiber. Interestingly, we have previously reported that the combination of these biomarkers identifies patients with heart failure presenting with a complex pattern of MIF characterized by both increased CCL and CD (CCL+CD+) showing a higher risk of adverse clinical evolution as compared with heart failure patients without this combination of biomarkers. As both increased CCL and CD have been found in the left atrial myocardium in patients with AF, we designed this investigation to explore whether the CCL+CD+ combination of biomarkers is associated with AF. (more…)