Author Interviews, Surgical Research / 24.09.2018
Two Studies Evaluate OviTex Reinforced BioScaffolds for Hernia and Soft Tissue Repair
MedicalResearch.com Interview with:
Maarten Persenaire, MD
Co-founder, Chief Medical Officer
TELA Bio
MedicalResearch.com: What is the background for this study? What are the main findings?
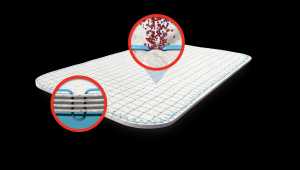
Response: OviTex Reinforced BioScaffolds (RBSs) are a novel distinct class of surgical implants that combine biologic and synthetic materials in a unique embroidered construction and design for hernia repair and soft tissue reconstruction. The two recent publications reported clinical results of OviTex RBS performance in inguinal and hiatal hernia repair.
Case series published in the International Journal of Surgery Open evaluated the role of OviTex RBSs in inguinal hernia repair to reduce the incidence of chronic postoperative pain. Thirty-one consecutive patients who had inguinal hernia repaired with OviTex RBSs were followed for an average of 12.6 months, during which time there were no reported recurrences, complications requiring surgical intervention or infections. None of the patients reported postoperative inguinal pain beyond the first days after surgery and none required a narcotic pain medication refill.
The second study published in the Journal of the Society of Laparoendoscopic Surgeons is the first reported series describing the use of OviTex RBSs in hiatal hernia repair. A retrospective chart review of 25 consecutive patients undergoing laparoscopic or open hiatal hernia repairs with mean follow-up of 14.2 months showed no recurrences. The hiatal hernia repairs with OviTex RBSs resulted in good to excellent control and resolution of symptoms, including heartburn, dysphagia, regurgitation, nausea and vomiting, dyspnea, and chest pain or discomfort. (more…)