MedicalResearch.com Interview with:
Rakesh K. Jain, Ph.D.
MedicalResearch.com Interview with:
Rakesh K. Jain, Ph.D.
A.W.Cook Professor of Tumor Biology
Director, E.L. Steele Laboratory
Department of Radiation Oncology
Harvard Medical School and
Massachusetts General Hospital Boston, MA 02114
Medical Research: What are the primary findings of this study and why are they important?
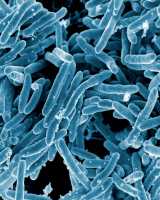
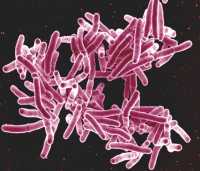
Dr. Jain: Pulmonary granulomas are the hallmark of the Tuberculosis (TB) infection, yet it is not fully understood how these structures contribute to disease progression and treatment resistance. In this study, we applied our insight in tumor biology – gained over three decades – to explore and exploit the similarities between vasculature (blood vessel network) in solid cancerous tumors and TB pulmonary granulomas. We demonstrate for the first time that TB granulomas have abnormal vasculature. This abnormality provides a mechanism for the observation that TB granulomas are often hypoxic (have low oxygen conditions) and have differential distribution of anti-TB drugs. We showed that bevacizumab, a widely prescribed anti-VEGF antibody for cancer and eye diseases, is able to create more structurally and functionally normal granuloma vasculature and improve small molecule delivery. This study suggests that vasculature normalization in combination with anti-TB drugs has the potential to enhance treatment in patients with TB.
Tuberculosis (TB) is a global scourge that is responsible for nearly 2 million deaths annually. Due to the inability of currently available treatment regimens to eradicate this devastating disease, it is clear that new treatment strategies are urgently needed. Unlike many researchers in the TB field, we
do not seek to discover new therapeutics that target
bacterial resistance; instead, we strive to overcome
physiological resistance to treatment resulting from abnormalities in the granuloma vasculature that impair drug delivery and create hypoxia that impairs efficacy of drugs and immune system. By using an FDA-approved drug, our study has the potential to be rapidly translated into the clinic.
Medical Research: Has any association previously been made between the vascular structure of TB granulomas and the challenges of treating TB – both the fact that treatment takes so long and the development of multidrug resistance?
Dr. Jain: Our study is the first to implicate a specific facet of the granuloma – the abnormal vasculature – as a potential contributor to disease progression and treatment resistance. Granuloma hypoxia is known to negatively affect the local immune system while conferring resistance to some of the TB drugs. Our collaborators have shown that different anti-TB drugs have differential abilities to penetrate the granuloma structure, especially to the interior granuloma regions where the
TB bacteria are found in greatest numbers. Our study is the first to provide evidence that by modulating the granuloma vasculature, hypoxia can be alleviated and drug delivery can be improved.
(more…)