10 Sep Adolescents Face Large Addiction-Treatment Gap
MedicalResearch.com Interview with:
Scott E. Hadland, MD, MPH, MS
Assistant Professor of Pediatrics
Boston Medical Center / Boston University School of Medicine
MedicalResearch.com: What is the background for this study?
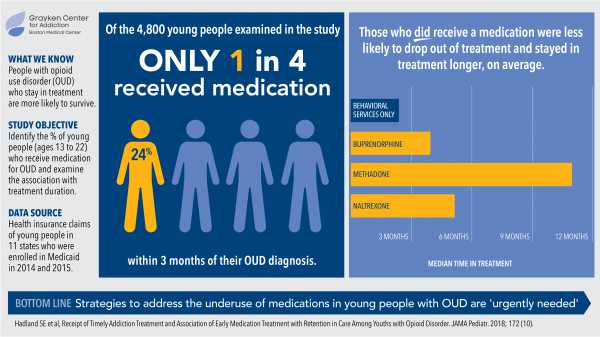
Response: Amidst a worsening overdose epidemic in the United States, adolescents and young adults have not been spared. Although evidence-based medications like buprenorphine, naltrexone, and methadone are recommended for adolescents and young adults, the extent to which youth receive these medications — and whether these medications help retain youth in addiction treatment — isn’t yet known.
MedicalResearch.com:? What are the main findings?
Response: We studied Medicaid-enrolled youth aged 13-22 from 11 US states and identified approximately 4800 youth diagnosed with opioid use disorder between 2014-2015. Even after being diagnosed and presenting for care, only 1 in 4 youth overall received an evidence-based medication. This gap was substantially larger for adolescents, among whom only 1 in 21 received a medication. Most youth received only behavioral health services (e.g., counseling, group therapy) for treatment.
Yet, when youth received medications, they were more likely to remain engaged in treatment. Youth receiving only behavioral health services typically left treatment early after only 67 days. However, youth receiving buprenorphine typically stayed in treatment 123 days; naltrexone, 150 days; and methadone, 324 days.
So, our results show that youth are at once unlikely to receive evidence-based treatment and more likely to be retained in care when they do.
MedicalResearch.com: What should readers take away from your report?
Response: Readers should know that there is a large addiction treatment gap for young people, and also that medications for addiction treatment are effective and, based on our study, help keep youth engaged in care. That many youth do not receive the standard of care flies in the face of current clinical guidelines from the American Academy of Pediatrics and the American Society of Addiction Medicine, among other national bodies, all of whom recommend that young people receive the same evidence-based treatment as adults do.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Future work should determine the extent to which the improvement we saw in retention in care was due to the medications themselves vs. the systems of care in which they are delivered. For example, it is known that buprenorphine is a highly effective treatment for opioid addiction. Yet, it is additionally possible that treatment programs that offer buprenorphine provide higher quality care than treatment programs that do not offer it (since treatment programs offering buprenorphine are adhering to national standards of care).
No disclosures
Citation:
[wysija_form id=”3″]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on September 10, 2018 by Marie Benz MD FAAD