28 Jun Common Diuretic HCTZ Associated With Increase Risk of Skin Cancers
MedicalResearch.com Interview with:
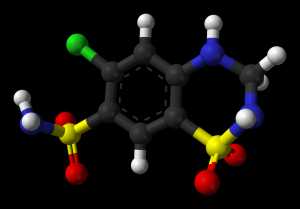
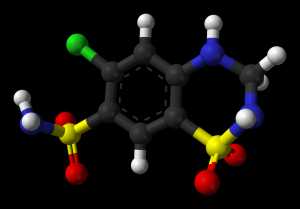
“Hydrochlorothiazide (HCTZ or HCT) is a diuretic medication often used to treat high blood pressure and swelling due to fluid build up” – Wikipedia
Sidsel Arnspang Pedersen MD
Department of Public Health, Clinical Pharmacology and Pharmacy
Anton Pottegård PhD
Associate professor, Clinical Pharmacy
Odense University Hospital
University of Southern Denmark,
The following is based on results from three published papers in JAAD and JAMA Internal Medicine. (1–3)
MedicalResearch.com: What is the background for this study?
Response: Hydrochlorothiazide is one of the most frequently used diuretic and antihypertensive drugs in the United States and Western Europe. The drug is known to be photosensitizing and has previously been linked to lip cancer.4–6 Based on these previous findings, the International Agency for Research on Cancer (IARC) has classified hydrochlorothiazide as ‘possibly carcinogenic to humans’ (class 2B).
This prompted us to investigate whether use of hydrochlorothiazide was associated to other UV dependent skin cancers, including non-melanoma skin cancer (i.e. basal cell carcinoma (BCC) and squamous cell carcinoma (SCC)), cutaneous melanoma, as well as the more rare non-melanoma skin cancers Merkel cell carcinoma and malignant adnexal skin tumours.
MedicalResearch.com: What are the main findings?
Response: We found a striking association between use of hydrochlorothiazide and risk of squamous cell carcinoma, with a steep dose-response pattern, with odds ratios (ORs) reaching 7.38 (6.32-8.60) with cumulative use of ≥200,000 mg hydrochlorothiazide. A weak dose-dependent association was seen for BCC, with an OR of 1.54 (1.38-1.71) associated with cumulative use of ≥200 000 mg hydrochlorothiazide. For melanoma, we found an association of 1.22 (1.09-1.36) with hydrochlorothiazide use (≥50 000mg), driven by increased ORs for nodular 2.05 (1.54-2.72) and lentigo melanoma 1.61 (1.03-2.50). ORs for Merkel cell carcinoma and malignant adnexal skin tumours associated with highest use (≥100,000mg) of hydrochlorothiazide were 3.3 (1.3-8.3) and 5.6 (2.4-13.3), respectively.
MedicalResearch.com: What should readers take away from your report?
Response: It seems that hydrochlorothiazide is associated with increased risk for all UV dependent skin cancers. The most striking association is seen with squamous cell carcinoma. However, we also observed associations to rarer types of skin cancer (certain subtypes of melanoma, Merkel cell carcinoma and malignant adnexal skin tumours). An important take home message, however. is that the increase in absolute risk of any of the skin cancers mentioned above is still very small for the single patient. Acknowledging the well-documented benefits of using hydrochlorothiazide, it is important to emphasize that any changes in antihypertensive therapy should only be performed in consultation with the doctor responsible for the patient.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Our findings have already resulted in attention from the European Medicines Agency (EMA), and the US Food and Drug Administration (FDA). Our study results have been evaluated in the Pharmacoviligance Risk Assesment Committee (PRAC), within the EMA.7 While they are reviewing the new findings, other studies are currently being mounted, looking to replicate the findings in other populations.
MedicalResearch.com: Is there anything else you would like to add?
Response: Anton Pottegård has participated in research projects unrelated to the present study using grants provided by LEO Pharma (manufacturer of bendroflumethiazide (another photosensitizing thiazide-diuretic)) to the institution where he was employed. The remaining authors declare no relevant conflicts of interest.
Citations:
1. Pedersen SA, Gaist D, Schmidt SAJ, Hölmich LR, Friis S, Pottegård A. Hydrochlorothiazide use and risk of nonmelanoma skin cancer: A nationwide case-control study from Denmark. Journal of the American Academy of Dermatology. 2018;78(4):673-681.e9. doi:10.1016/j.jaad.2017.11.042
2. Pottegård A, Pedersen SA, Schmidt SAJ, Hölmich LR, Friis S, Gaist D. Association of Hydrochlorothiazide Use and Risk of Malignant Melanoma. JAMA Internal Medicine.
3. Pedersen SA, Schmidt SAJ, Hölmich LR, Friis S, Pottegård A, Gaist D. Hydrochlorothiazide use and risk of Merkel cell carcinoma and malignant adnexal skin tumors: A nationwide case-control study. Journal of the American Academy of Dermatology. 2018;0(0). doi:10.1016/j.jaad.2018.06.014
4. Pottegård A, Friis S, Christensen R dePont, Habel LA, Gagne JJ, Hallas J. Identification of Associations Between Prescribed Medications and Cancer: A Nationwide Screening Study. EBioMedicine. 2016;7:73-79. doi:10.1016/j.ebiom.2016.03.018
5. Friedman GD, Asgari MM, Warton EM, Chan J, Habel LA. Antihypertensive drugs and lip cancer in non-Hispanic whites. Arch Intern Med. 2012;172(16):1246-1251. doi:10.1001/archinternmed.2012.2754
6. Pottegård A, Hallas J, Olesen M, et al. Hydrochlorothiazide use is strongly associated with risk of lip cancer. Journal of Internal Medicine. June 2017. doi:10.1111/joim.12629
7. Pharmacoviligance Risk Assessment Committee (PRAC) January 2018. http://www.ema.europa.eu/docs/en_GB/document_library/Minutes/2018/03/WC500244940.pdf.
[wysija_form id=”3″]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on June 28, 2018 by Marie Benz MD FAAD
